Cancer research is no longer inching forward; rather, it is accelerating at lightning speed. In 2025, we are witnessing a new era in oncology, where science is not only keeping pace with cancer but, in many cases, outrunning it.
Thanks to incredible breakthroughs in immunotherapy and early cancer detection, what once felt like science fiction is now saving lives across the globe. From blood tests that spot cancer before symptoms appear, to treatments that empower the immune system to destroy tumors, the future of cancer care is here, and it is nothing short of extraordinary!
Across labs, clinics, and global research hubs, the world’s brightest minds are joining forces with one goal – to detect cancer earlier, treat it smarter, and give patients longer, healthier lives.
In this blog, we proudly spotlight the most recent, life-changing cancer breakthroughs in immunotherapy and early detection.
Worldwide Breakthroughs in Cancer Immunotherapy Unveiled
So far this year, three landmark studies have pushed the boundaries of what is possible in cancer immunotherapy. Take a look:
#1 Fred Hutch Study Uncovers Natural Boosters for Immunotherapy
A new study from the Fred Hutchinson Cancer Center revealed that certain autoantibodies naturally present in some cancer patients can significantly enhance the effectiveness of checkpoint inhibitors. These autoantibodies appear to “prime” the immune system, helping it recognize and attack tumor cells more aggressively.
When present, researchers observed that these immune-enhancing antibodies could make cancer immunotherapy 5 to 10 times more effective in reducing tumor size compared to patients without them.
What to expect: This discovery could pave the way for personalized immunotherapy screening. Which means, a patient’s antibody profile will be used to predict his/her likelihood of responding to treatment, marking a major step toward precision oncology.
#2 New Study Shows Radiation Makes Cold Tumors More Responsive to Immunotherapy
In a major July 2025 cancer breakthrough published in Nature Cancer, researchers led by Johns Hopkins University have shown that combining radiation therapy with immunotherapy can dramatically improve treatment outcomes for certain hard-to-treat cancers. Specifically, the study focused on “cold” lung tumors that traditionally evade immune detection and are resistant to immunotherapy alone.
The research team found that administering radiation first helps recondition the tumor microenvironment, essentially making it more visible and vulnerable to immune system attack. Once “warmed up,” these tumors become more immunogenic, allowing checkpoint inhibitors or other cancer immunotherapy drugs to work more effectively.
This combined approach not only led to local tumor shrinkage but also triggered systemic anti-tumor immune responses, reducing metastases in distant parts of the body. In essence, the study provides compelling evidence that sequencing radiation before immunotherapy cancer treatment could unlock powerful new treatment combinations – especially for patients who previously had limited options.
What to expect: This research could reshape protocols for treating non-small cell lung cancer and potentially other “cold” tumors across cancer types.
#3 AI-Engineered Immune Proteins Usher in New Era of Precision Oncology
In a groundbreaking advancement, researchers have introduced an AI-powered platform that can design custom immune-modulating proteins within a matter of weeks. Whereas the traditionally takes years to use conventional drug development pipelines. This system, built on innovative machine learning algorithms, can generate synthetic proteins that train a patient’s immune system to recognize and attack tumors with higher precision.
These engineered proteins act as biological “weapons,” essentially priming the patient’s own immune cells to home in on cancerous targets more effectively. Unlike traditional immunotherapies that rely on generalized mechanisms, this approach allows for ultra-specific personalization, accounting for individual tumor signatures and patient immune variability.
The AI platform works by analyzing massive datasets of protein interactions, immune responses, and tumor microenvironment factors, then rapidly predicting the optimal therapeutic design for a given patient’s profile. Early-stage studies have shown remarkable promise in both solid tumors and hematologic malignancies.
What to Expect: This innovation could reshape the entire cancer immunotherapy development process, slashing time and cost while vastly improving patient-matching accuracy. Oncologists may soon gain access to AI-generated treatment blueprints, enabling highly individualized therapy plans based on a patient’s unique immune landscape.
It’s a step closer to on-demand, algorithm-driven cancer care, where therapies are not just targeted but tailored in real time.
A New Era of Early Cancer Detection Has Begun!

Researchers and health systems worldwide are converging on one goal: detecting cancer before symptoms appear. Here are a few breakthrough cancer detection updates that have taken place recently:
#1 PAC‑MANN Test Shows Promise for Early Pancreatic Cancer Detection
In a major leap for early cancer diagnostics, researchers from Oregon Health & Science University (OHSU) have unveiled a novel blood test – PAC‑MANN (Protease Activity-based Assay using a Magnetic Nanoparticle). This blood test could significantly improve pancreatic cancer early detection, one of the deadliest and most elusive malignancies.
The test, published in Science Advances, uses magnetic nanosensors to detect specific protease activity (enzymes linked to tumor growth) directly from a single drop of blood. The result is a noninvasive, affordable, and scalable tool that could transform how and when pancreatic cancer is diagnosed.
Key Findings:
- 73% overall sensitivity in detecting pancreatic ductal adenocarcinoma (PDAC).
- When combined with the standard CA 19‑9 biomarker, detection accuracy rose to 85% in Stage I patients.
- 98% specificity, meaning extremely low false-positive rates.
- The test can be completed in under an hour and costs less than 1 cent.
What to Expect: PAC‑MANN is undergoing further clinical validation. But its potential is already clear – it could become a frontline tool for early cancer detection in high-risk populations, especially where advanced imaging is unavailable. With its low cost and ease of use, this test could make early detection accessible globally, including in low-resource or rural settings. In short, this could be a game-changer for a type of cancer that is often caught too late.
#2 miONCO‑Dx: AI‑Powered Blood Test Detects 12 Cancers at 99% Accuracy
Researchers at the University of Southampton, UK, in collaboration with biotech firm Xgenera and funded by the National Institute for Health and Care Research (NIHR), have developed miONCO‑Dx. This is an AI‑driven blood test that analyzes microRNA in just a few drops of blood to detect 12 common cancers, such as – including bowel, lung, breast, and pancreatic cancers. Initial validation on data from 20,000 patients showed over 99% accuracy, with nearly perfect sensitivity and specificity.
A £2.4 million grant has been awarded to support real-world clinical trials involving 8,000 NHS patients, a key step toward making this test available through routine care.
What to expect: If approved, miONCO‑Dx could significantly improve early cancer detection, save lives, and reduce healthcare resource strain across the NHS.
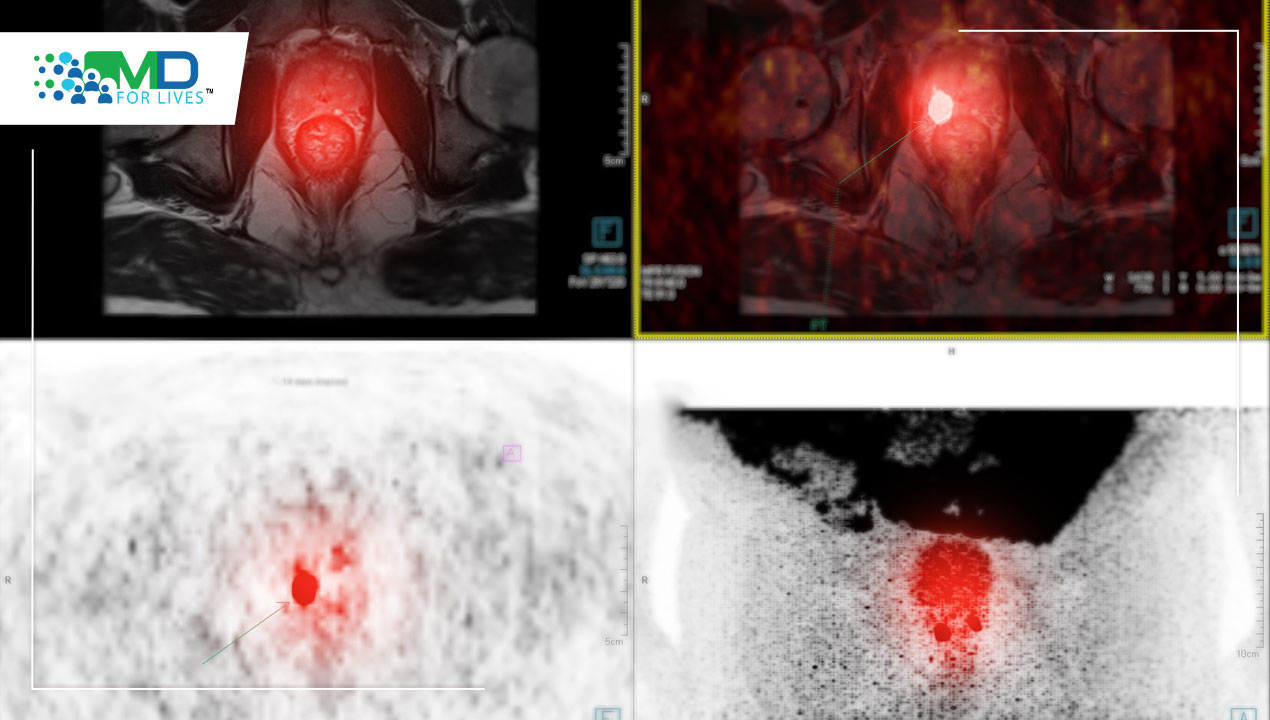
#3 Germany Launches National Low-Dose CT Lung Cancer Screening Program
Germany has officially launched its first structured national lung cancer screening program using low-dose CT (LDCT) targeting high-risk individuals (ages 50–75, current or former heavy smokers). This initiative is grounded in the Lung Cancer Early Detection Ordinance issued by the Federal Ministry for the Environment, Nature Conservation, Nuclear Safety and Consumer Protection.
The program mandates double reading of all CT scans and sets stringent quality control standards for lung cancer early detection. It also requires follow-up review by specialized radiologists for any suspicious findings, ensuring adherence to high diagnostic accuracy and patient safety. The Federal Joint Committee (G‑BA) is now evaluating how the program will be incorporated into statutory health insurance coverage and what specific guidelines will be implemented.
What to expect: Germany’s LDCT screening program places it among leading countries committed to lung cancer early detection, such as the U.S., Canada, and South Korea. By proactively targeting high-risk groups and ensuring exam precision, this rollout could significantly reduce lung cancer mortality rates while minimizing overdiagnosis risks.
Why Look Elsewhere, When It All Comes to You Here?
In an era of overwhelming information, not every headline is worth your attention. But here, we cut through the noise, bringing you only the most credible, meaningful, and timely cancer breakthroughs from around the world – whether it’s related to immunotherapy, or early cancer detection.
No chasing updates across scattered sources. Just one destination, always ahead of the curve.
Want to do more than just stay informed? Join MDForLives and contribute directly to the kind of global medical research shaping these very headlines. Register today to share your medical expertise, earn rewards, and collaborate with world-renowned researchers driving the future of healthcare.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.