Glioblastoma (GBM), one of the most fatal forms of cancer, evokes a sense of fear and dread in any patient suffering from it. Buried deep within the brain, this perilous disease reappears 90% of the time, shattering the fragile hope that often follows the initial treatment.
But amidst the despair, there’s hope.
Advancements in glioblastoma research have provided a growing number of treatment options, each aimed at battling this deadly cancerous tumor. Although surgery remains a fundamental approach, aiming to remove the tumor completely, glioblastoma’s diffusive nature and its ability to infiltrate healthy brain tissues can make complete resection challenging.
This is where CAR T cell therapy emerges as a more promising and effective treatment option.
In an effort to assess the perspective of various neurosurgeons on dual-target CAR T cell therapy for recurrent glioblastoma (GBM), MDForLives curated a survey, and the findings are quite insightful.
80% OF NEUROSURGEONS SAY: “SURGERY IS THE FIRST LINE OF DEFENSE”
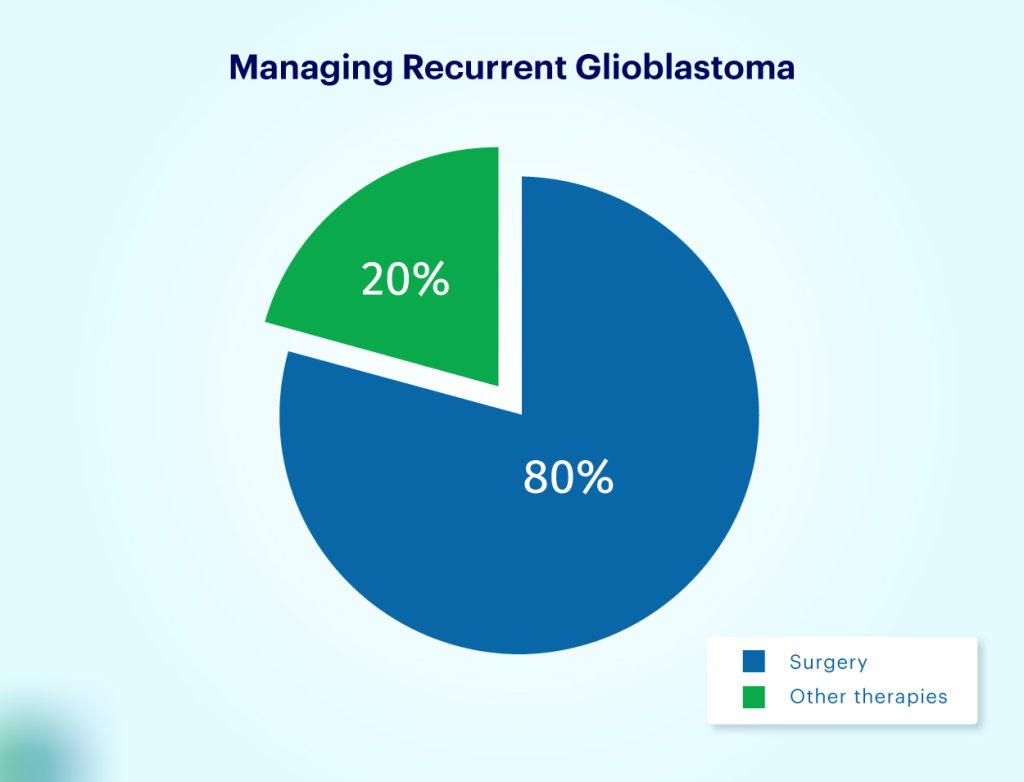 Our recent survey across the US, Canada, and the UK shows that surgery remains the most common approach to treating recurrent glioblastoma cases. 80% of respondents have reported choosing surgery over:
Our recent survey across the US, Canada, and the UK shows that surgery remains the most common approach to treating recurrent glioblastoma cases. 80% of respondents have reported choosing surgery over:
- Chemotherapy
- Radiation therapy
- Cancer Immunotherapy
- Palliative Care
However, in the case of glioblastoma surgery, the primary goal is to excise the cancerous tissue while sparing the surrounding healthy brain tissue, which is crucial for preserving the patient’s neurological functions. Since the brain is the control center for all our bodily functions, even minor damage during surgery can have devastating consequences.
Therefore, surgeons prioritize maximizing the patient’s neurological function by preserving healthy brain tissue, even if it means leaving some tumor cells behind. This is a major limitation of surgery in treating glioblastoma.
CAR T CELL THERAPY: THE NEXT FRONTIER IN RECURRENT GLIOBLASTOMA TREATMENT
As a new challenger in the fight against recurrent glioblastoma, CAR T cell therapy involves genetically modifying a patient’s T cells to target and eliminate tumor cells. The cutting-edge treatment includes extracting T cells from the patient, engineering them in the laboratory to express Chimeric Antigen Receptors (CARs) specific to glioblastoma cells, and then reinfusing these modified cells back into the patient.
Early clinical trials of CAR T cell therapy have shown encouraging results, with some patients experiencing significant tumor reduction and improved survival rates. The precision in this approach allows the modified T cells to specifically target cancer cells, minimizing damage to healthy tissues and reducing the side effects commonly associated with traditional treatments.
NEUROSURGEONS’ TAKE ON CAR T CELL THERAPY
The responses received from our panelists (Neurosurgeons) are a combination of “yes” and “maybes.” However, the good news is that not a single surgeon has denied the power of CAR T Cell Therapy or opposed its use.
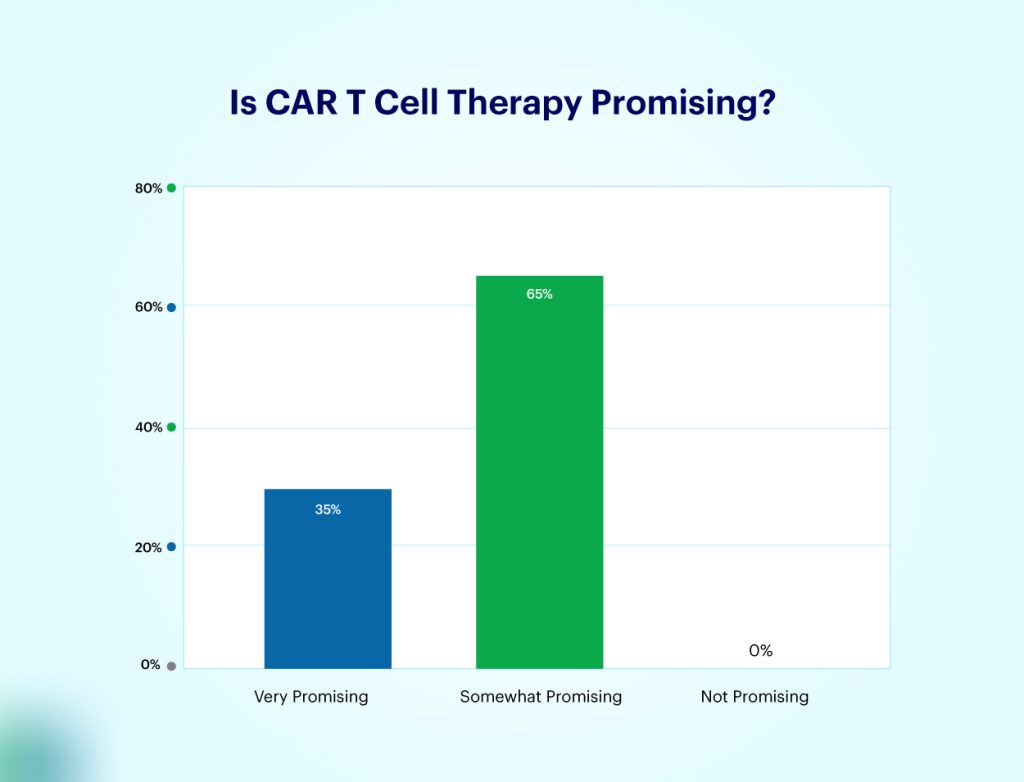
Most neurosurgeons are still unsure about using this therapy because medical researchers have yet to establish the long-term effectiveness and safety profile of CAR T cell therapy for glioblastoma recurrence.
Researchers are currently busy addressing challenges such as the tumor’s ability to evade the immune system, and the potential severe side effects of the therapy. Additionally, efforts are being made to refine the technology to enhance its accessibility and affordability for a broader range of patients.
REMEMBER, THE FIGHT CONTINUES!
Recurrent glioblastoma is still considered one of the most fatal medical conditions, but thankfully, neuro-oncology is constantly evolving. The emergence of CAR T cell therapy, while still in its nascent stages, offers a promising new avenue for treatment. As long as medical researchers continue their research alongside surgical resection or established therapies like chemotherapy and radiation, neurosurgeons are better equipped to fight this lethal form of cancer.
If you are a neurosurgeon who has dealt with cases related to glioblastoma recurrence, share your story with us at collaboration@mdforlives.com.
To gain more insights and become a part of a community of skilled surgeons, join us now!

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.