Alzheimer’s disease is a complex condition that affects millions of people worldwide. Alzheimer disease (AD) is a crucial area of study in biomedicine. Amyloid beta (Aβ) deposition, neurofibrillary tangles, neuroinflammation, synaptic degeneration, and neuronal loss are key pathological characteristics of AD. The main clinical manifestation of AD is the progressive decline of cognitive function and activities of daily living. While researchers have made significant progress in understanding the disease, there are still many controversies and debates in the field. Some of the most significant contradictions in Alzheimer’s research are discussed below:
1. Amyloid Hypothesis:
The amyloid hypothesis suggests that the accumulation of amyloid-beta (Aβ) peptide in the brain is the primary cause of AD. However, this hypothesis has been challenged by several studies that have failed to show a clear link between Aβ accumulation and cognitive decline. Additionally, some researchers have proposed that Aβ accumulation may be a downstream effect of other pathological processes in AD.
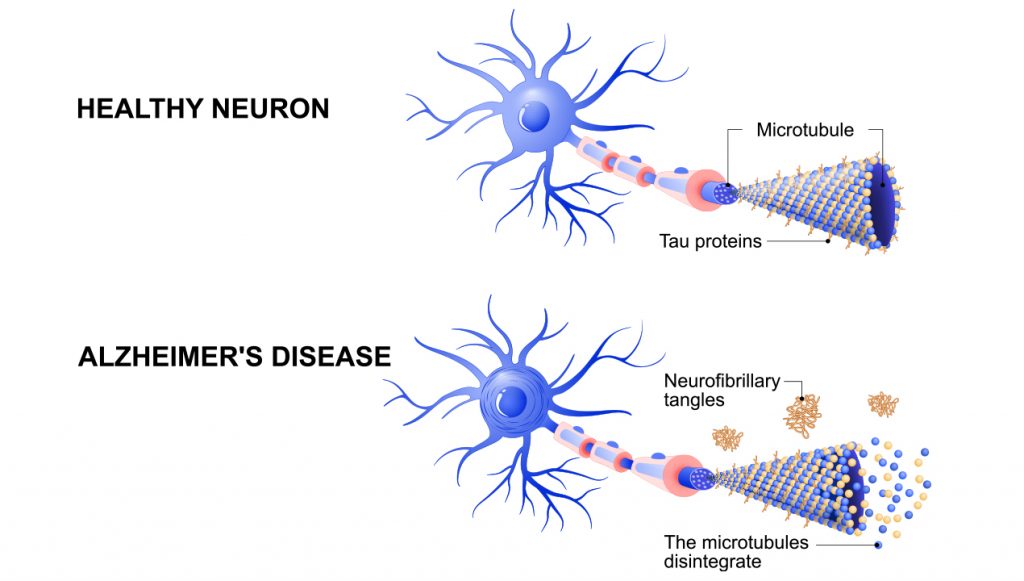
2. Tau hypothesis:
The tau hypothesis suggests that the accumulation of tau protein in the brain is the primary cause of AD. However, the role of tau in AD pathogenesis is still not fully understood, and there is evidence to suggest that both Aβ and tau may contribute to AD pathology.
3. Diagnosis:
AD is typically diagnosed based on clinical symptoms and cognitive testing, but there is skepticism about the accuracy of these diagnostic methods. Some researchers have proposed the use of biomarkers, such as Aβ and tau levels in cerebrospinal fluid or neuroimaging techniques, to aid in the diagnosis, but there is still debate over the best diagnostic approach.
4. Genetic Risk Factors
There is evidence to suggest that genetic factors play a role in the development of Alzheimer’s disease. The genetic association provides a solid foundation for furthering the understanding of the etiology of this complex disease. Over 50 genes have now been linked to Alzheimer’s disease, indicating that the disease has multiple components, as supported by pathway analyses (immunity, endocytosis, cholesterol transport, ubiquitination, amyloid-β, and tau processing). Over half of late-onset Alzheimer’s heritability has been identified, allowing researchers to calculate the accumulation of AD genetic risk using polygenic risk scores. However, there is still debate about which genes are most important and how they interact with environmental factors.
5. Role of Inflammation
Since the 1980s, the presence of immune-related antigens and cells around amyloid plaques in the brains of Alzheimer’s disease (AD) patients has been reported, in addition to amyloid beta and tau protein aggregates. Additional findings of activated complement factors, cytokines, and a wide range of related receptors in the brains of Alzheimer’s disease patients in the 1990s led to the concept of neuroinflammation (inflammation within the central nervous system (CNS)), which suggests that immunological processes in the brain are likely to be involved in the pathology of CNS degenerative diseases. The inflammation hypothesis emerged only recently when it became clear that the observations of altered immune processes in Alzheimer’s disease could not be ignored. Inflammation has been implicated in the development of Alzheimer’s disease, but the extent to which it contributes to the disease is still unclear. Some researchers argue that inflammation is a secondary factor that exacerbates the disease, while others suggest that it may be a primary cause.
6. Link Between Alzheimer’s Disease and Diabetes
There is evidence to suggest that there is a link between Alzheimer’s disease and diabetes, with some researchers proposing that the two conditions may share common underlying mechanisms. The pathophysiology of Alzheimer’s disease heavily relies on the amyloid cascade. Amyloid beta peptides build up over time, causing tau proteins to become hyperphosphorylated and form neurofibrillary tangles, which cause neurodegeneration and cerebral atrophy. Aside from these processes, the altered glucose metabolism and insulin signaling in the brain during Alzheimer’s disease appear to cause early neuronal loss and synaptic plasticity impairment, years before the clinical manifestation of the disease. The presence of insulin resistance in the brain during Alzheimer’s disease has led to the disease being referred to as “Type 3 diabetes”. However, this link is still not fully understood, and the precise nature of the relationship between the two conditions remains a topic of debate.
7. Can Alzheimer’s Disease be Prevented?
Finally, there is a debate about whether Alzheimer’s disease can be prevented or not, and if so, how. The average survival time for an Alzheimer’s disease patient is 4 to 6 years after diagnosis; however, survival time can be as long as 20 years from the onset of initial symptoms, which can appear in the 30s, 40s, and beyond. This window of opportunity implies that many people can live longer lives by making life-changing decisions about diet, exercise, nutritional supplements, and nutraceuticals. While some researchers are optimistic about the potential for lifestyle interventions and early detection to prevent the disease, others are more cautious, arguing that the underlying causes of the disease are still not fully understood.
References:
- Inflammation in Alzheimer’s disease: relevance to pathogenesis and therapy. Alzheimer’s Research & Therapy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2874260/. Accessed 2/22/2023
- The multiplex model of the genetics of Alzheimer’s disease. nature neuroscience. https://www.nature.com/articles/s41593-020-0599-5#:~:text=Abstract,onset%20AD%20showing%20over%2090%25. Accessed 2/22/2023
- The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Molecular Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4888851/#:~:text=Amyloid%20imaging%20and%20CSF%20biomarkers&text=Initial%20analyses%20of%20a%20familial,Bateman%20et%20al%2C%202012). Accessed 2/22/2023
- Current Alzheimer disease research highlights: evidence for novel risk factors. Chinese Medical Journal. https://journals.lww.com/cmj/fulltext/2021/09200/current_alzheimer_disease_research_highlights_.3.aspx. Accessed 2/22/2023
- Type 2 Diabetes Mellitus and Alzheimer’s Disease: Shared Molecular Mechanisms and Potential Common Therapeutic Targets. International Journal of Molecular Sciences. https://www.mdpi.com/1422-0067/23/23/15287/pdf#:~:text=Numerous%20epidemiological%20data%20suggest%20that,the%20pathophysiology%20of%20Alzheimer’s%20disease. Accessed 2/22/2023
- Can Alzheimer Disease Be Prevented? Intractable & rare diseases research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204553/. Accessed 2/22/2023

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.






