Infection management continues to be one of the most pressing and complex challenges in cancer care. Cancer patients, especially those undergoing chemotherapy, radiotherapy, or hematopoietic stem cell transplantation, often experience profound immunosuppression leading to cancer infection. For these patients, even a short delay in starting treatment can mean the difference between recovery and rapid deterioration. At the same time, unnecessary or prolonged antimicrobial use carries its own risks. This includes – toxicity, disruption of the microbiome, and the growing global crisis of antimicrobial resistance (AMR).
This clinical tightrope places oncologists and critical care specialists in a constant dilemma. They often ask themselves – “Should treatment start right away based on suspicion (Empirical Therapy)?” “Or, should we wait for early signs or biomarkers (Preemptive Treatment)?” Each approach comes with trade-offs. Empirical treatment maximizes speed but may contribute to overtreatment and resistance. Whereas, on the other hand, preemptive treatment offers a more targeted strategy but risks missing the critical window for timely intervention.
Striking the right balance between prompt action, patient safety, and responsible antimicrobial stewardship has become a defining question in modern cancer care. And as new diagnostics, biomarkers, and evolving treatment guidelines reshape practice, oncologists are increasingly reevaluating how best to approach this decision.
Our recent survey insights from over 8000 oncologists shed light on how these strategies are understood, applied, and perceived in real-world clinical settings. Keep reading!
What Is Empirical Therapy and Preemptive Treatment?
At the heart of cancer infection management lies a critical choice between speed and precision. Oncologists must decide whether to treat immediately, prioritizing rapid action, or to wait for early indicators that guide a more targeted approach. Understanding the differences between these two strategies is essential to evaluating their impact on patient outcomes.
- Empirical Therapy: Treatment begins right away based on clinical suspicion of infection, even before lab confirmation. This approach is often lifesaving in critically ill or immunocompromised patients, where even a short delay can worsen outcomes.
- Preemptive Treatment: In this case, the treatment starts only when early warning signs, biomarkers, or risk indicators point to an infection before the disease fully manifests. This strategy helps reduce unnecessary antimicrobial exposure and the risk of resistance.
Both approaches carry value, but their application often depends on patient condition, institutional protocols, and a physician’s clinical judgment.
How Familiar Are Oncologists with Empirical and Preemptive Treatment?
Awareness and understanding of preemptive and empirical treatment are already well embedded among oncologists. Our survey shows that familiarity levels are high across all regions (especially the US, UK, Italy and Canada), though the depth of engagement differs.
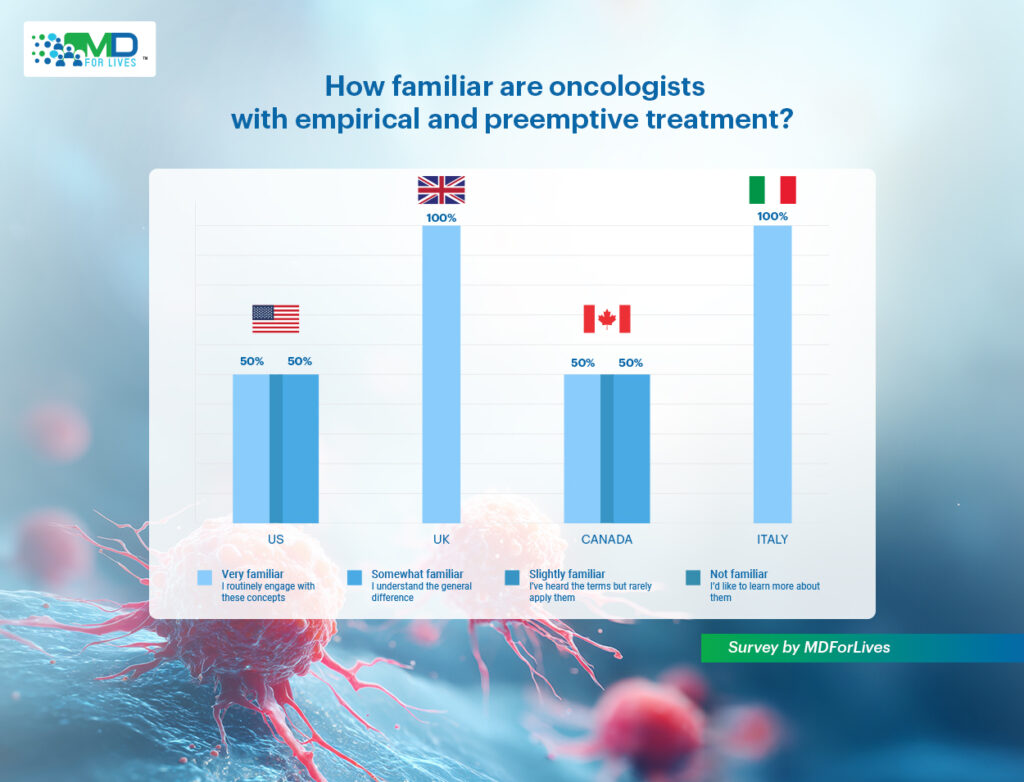
In the UK and Italy, oncologists reported 100% routine engagement with these therapies for cancer infection management, suggesting they are strongly integrated into everyday oncology practice and reinforced through national or institutional guidelines.
But in contrast, responses from the US and Canada reflected a more mixed picture. In both countries, half of the participants said they were “very familiar” and applied these concepts routinely, while the other half indicated they were only “somewhat familiar” acknowledging an understanding of the differences, but not always applying both approaches consistently in practice.
What stands out is that no respondents from any of the four big nations have reported being unfamiliar with these concepts. This strengthens the fact that both empirical and preemptive treatments have become core elements of cancer infection management, shaping how oncologists think about balancing rapid intervention with antimicrobial stewardship.
Antimicrobial Resistance: Which Approach Carries Greater Risk?
Among cancer patients, even the slightest complication, such as an infection, can escalate into a life-threatening emergency. The frequent reliance on broad-spectrum antimicrobials to protect immunocompromised individuals, while often necessary, creates fertile ground for the emergence of antimicrobial resistance (AMR). For oncologists and critical care teams, the decision between empirical and preemptive treatment is therefore not only about ensuring patient survival in the moment, but also about safeguarding the long-term effectiveness of these life-saving drugs.
Our survey responses reflect this delicate balance. Check out below.
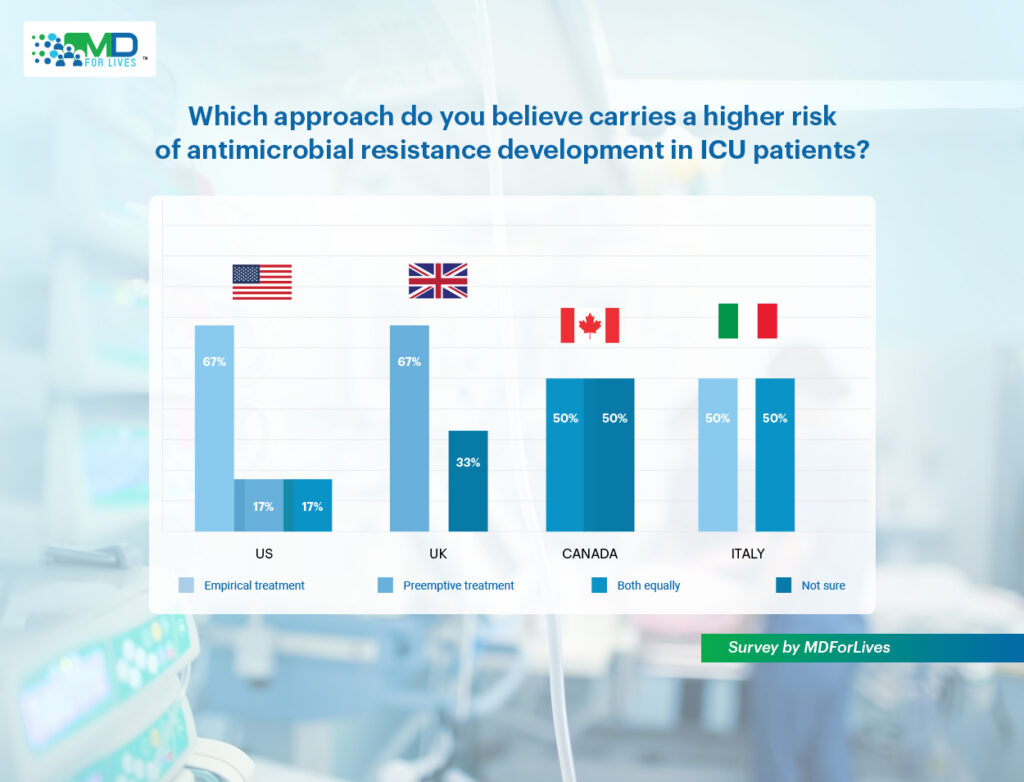
In the US, 67% of oncologists viewed empirical treatment as riskier. They worry about prescribing broad-spectrum antibiotics, before even test results are available. This can save lives, but it also risks overtreatment and speeds up resistance.
In contrast, UK respondents leaned the other way. Here, 67% perceived preemptive treatment as the greater risk. This perspective may be tied to the uncertainty surrounding biomarkers and early diagnostic signals. If these indicators are misinterpreted or lack strong validation, antimicrobials could be prescribed unnecessarily, again fueling resistance.
Elsewhere, views were more mixed. In Canada, half of respondents said both approaches carry equal risk, while others admitted they were unsure. Italian oncologists were also divided, with some pointing to empirical treatment as riskier and others highlighting that both strategies can be problematic depending on context.
These perspectives shed light on an important truth – the risk of resistance is less about which approach is chosen and more about how responsibly it is applied.
How Oncologists Weigh Safety in Cancer Infection Management
When asked which strategy better supports patient safety, oncologists were divided.

In the United States, a majority (83%) felt that both empirical and preemptive treatments have value depending on context. But here is the catch – 17% still leaned toward empirical treatment, emphasizing the urgency of immediate intervention in high-risk cancer patients.
In the UK, two-thirds of respondents (67%) also supported a balanced approach, while a third (33%) preferred preemptive treatment, pointing to its role in reducing unnecessary antimicrobial exposure. Canadian oncologists were split, with half favoring preemptive therapy and the other half considering both approaches equally valid.
In Italy, views were more evenly distributed: 50% supported empirical treatment for its life-saving speed, while the remaining 50% believed the best approach depends on the situation.
What do the findings suggest: Cancer infection management is rarely “one-size-fits-all.” The decision depends on multiple factors, including the patient’s condition, the availability of rapid diagnostics, and the treatment protocols followed at the institution.
Why Is Empirical Treatment Commonly Initiated?
Despite its risks, empirical treatment remains widely used, especially in Intensive Care Units (ICUs) treating cancer patients. The survey explored the reasons behind this reliance.
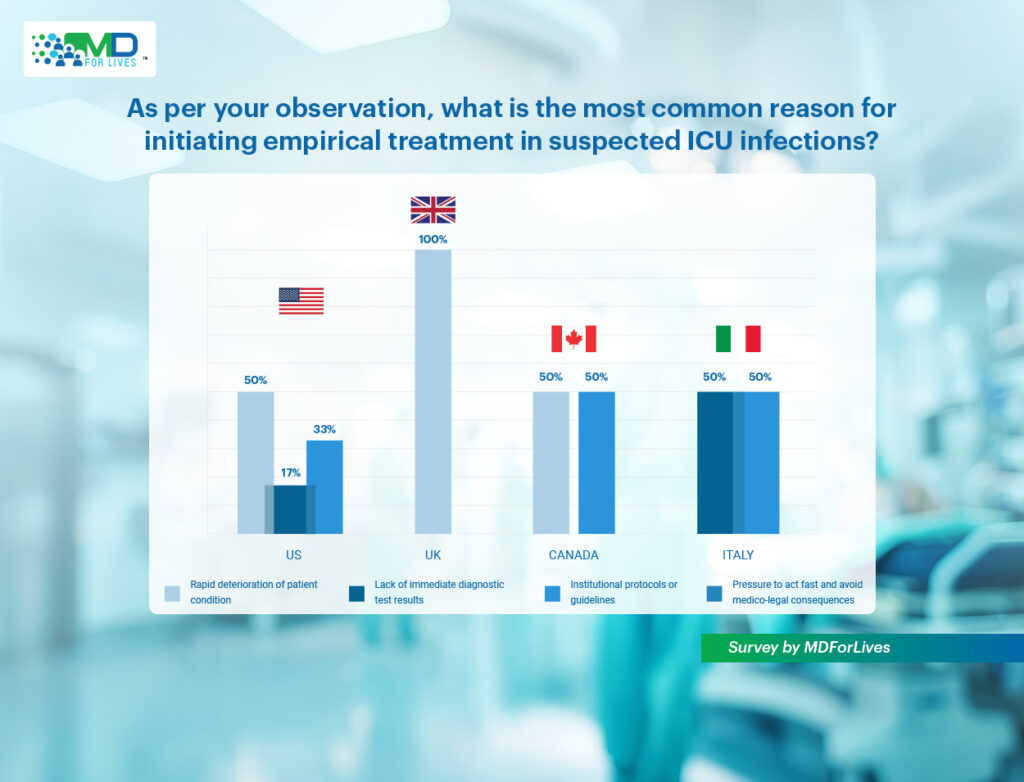
Across all regions, rapid patient deterioration emerged as the most common driver. Half of the US oncologists (50%) and all UK respondents (100%) cited it as the key factor, reflecting the urgency to act immediately when critically ill cancer patients show signs of infection. Canadian oncologists echoed this sentiment, with 50% also pointing to rapid clinical deterioration.
Institutional protocols and guidelines were another major influence. In the US, 33% of respondents found protocols as a reason for starting empirical treatment, with similar findings in Canada (50%) and Italy (50%). These built-in pathways recommend swift intervention for immunocompromised patients, underscoring the high stakes of oncology care.
Meanwhile, some oncologists noted the challenge of limited diagnostic access. In the US, 17% of oncologists raised this concern, as did 50% of Italian respondents. Without reliable test results available quickly, they felt compelled to start broad-spectrum coverage to avoid undertreatment.
Overall, the data highlights that empirical therapy often arises out of necessity rather than preference. For oncologists in both North America and Europe, the urgency of safeguarding patients in life-threatening situations often outweighs the long-term risks of overtreatment.
The Ongoing Dilemma in Oncology Care
The overall insights that we have gathered through our latest Oncology survey, brings to light a persistent dilemma that oncologists face:
- Act too soon (empirical treatment): Protects patients against sudden deterioration but increases antimicrobial use, resistance, and side effects.”
- Act too late (delayed preemptive treatment): The infection may worsen rapidly, leading to poor outcomes or even preventable mortality.
For oncologists, the decision is rarely straightforward. It is a delicate balance between life-saving urgency and long-term antimicrobial stewardship. Every choice carries trade-offs that affect not only the patient in front of them but also the broader effectiveness of antibiotics for future oncology patients.
The Path Forward: Smarter Strategies for Cancer Infection Control
To address this dilemma, oncologists and oncology researchers are exploring strategies that bring more precision into cancer infection management:
- Enhanced Diagnostics: Advances in rapid molecular tests and biomarker-based diagnostics could allow oncologists to move beyond “blind” empirical treatment, enabling earlier and accurate preemptive decisions.
- Adaptive Protocols: Hospitals can adopt hybrid approaches, starting with empirical therapy when necessary but rapidly de-escalating or tailoring treatment as soon as test results are available.
- Global Knowledge Exchange: Regional differences, such as the US seeing empirical therapy as riskier, versus the UK viewing preemptive treatment as the greater concern, highlight the need for shared best practices and international guidelines.
- Oncology-Specific Research: Oncologists and researchers urgently seek evidence on how these strategies affect cancer patients, who are especially vulnerable to infection and resistance.
Final Thoughts
Empirical or preemptive treatment? It is a question that does not have a simple answer, and it never will.
Cancer infection management is not about choosing one approach over the other. Rather, it is about understanding when and how each strategy should be applied. Empirical treatment may save a life when minutes matter, while preemptive treatment helps reduce unnecessary drug use and preserve antimicrobial power for the future. Both have merit, and both carry risks. The challenge lies in knowing which path to take with a vulnerable patient in front of you, and no time to second-guess.
What our oncology survey makes clear is that this dilemma is shaping cancer care globally. Oncologists across the US, UK, Canada and Italy are rethinking how to strike the right balance between immediate survival today and antimicrobial effectiveness tomorrow. The future may lie in smarter diagnostics, adaptive pathways, and shared global learning. Until then, the “empirical versus preemptive” debate will go on, it is the daily reality of oncologists working to keep their patients safe in the face of one of medicine’s toughest challenges.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.