Diabetes comes along with a higher risk for thrombosis. Research published in January 2022 points to a potential mechanism for this risk and could help doctors gain a better understanding of clotting susceptibility in the context of type 2 diabetes.
Diabetes and Thrombosis
According to the CDC, nearly 35 million Americans have type 2 diabetes mellitus (T2DM). Clot-related issues, along with cardiovascular complications in general, are the most common causes of death for people with T2DM. Prevention of thrombotic events in people with T2DM can include antithrombotic therapies as well as therapies aimed at controlling the glycemic dysfunction, dyslipidemia, and hypertension that are common in diabetes.

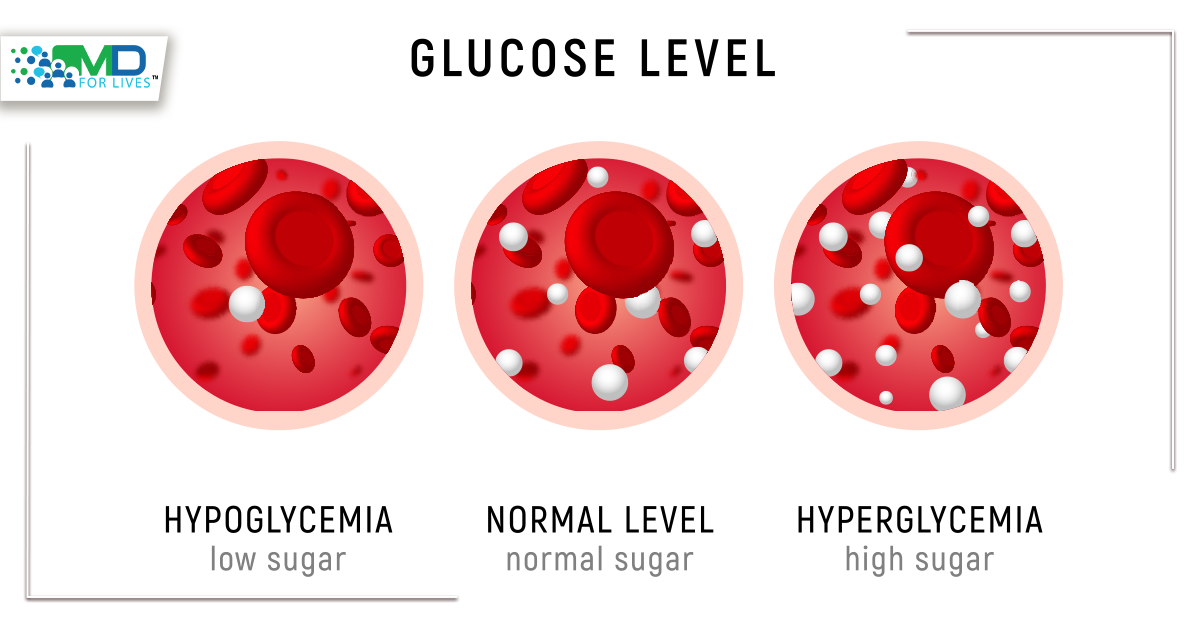
Signs of hyperglycemia
Signs of hyperglycemia (high blood glucose) can include thirst, frequent urination, headaches, difficulty concentrating, and blurred vision. If hyperglycemia is not kept under control, over time it can cause weight loss, susceptibility to infection, poor wound healing, gastrointestinal problems, nerve and vision damage, and cardiovascular complications.

In type 2 diabetics, hyperglycemia contributes to clotting risk by causing inflammation and oxidative stress, inducing platelet hyperreactivity, and triggering endothelial dysfunction. The mechanisms by which hyperglycemia leads to these problems are not fully understood but are under active research.
New Research Connects Clotting Risk to Hyperglycemia and Mechanical Stress
Mechanosensation, the ability of living things to sense and respond to mechanical forces, is a feature of almost all mammalian cells and is also found in living things as diverse as bacteria and plants. In the human bloodstream, red blood cells and platelets are exposed to mechanical forces and shear stress. These forces can change due to pathological conditions including vascular dysfunction seen in diabetes.
Research published in January 2022 and published in Science Translational Medicine shows that hyperglycemia changes the behavior of an ion channel called Piezo1, which responds to mechanical stimulation and shear stress, in hematopoietic lineage cells. Other recent research has linked the same ion channel to a wide variety of roles in cardiovascular health, inflammation, and immunity.
Piezo1 mechanoreceptors may contribute to clotting propensity in diabetes
The new research shows that Piezo1 is expressed at a higher level in the red blood cells, platelets, and neutrophils of type 2 diabetics, potentially making diabetics’ blood cells more sensitive to mechanical stress.
In laboratory tests, the researchers found that exposure to high glucose levels led to increased expression of Piezo1 ion channels on cells. The increased expression was seen both on mature white blood cells exposed to high glucose levels and on blood cells whose progenitors were exposed to high glucose levels during hematopoiesis. Moreover, hematopoietic stem cells with higher Piezo1 expression had a proliferative advantage when exposed to high glucose conditions.

The platelets of individuals with diabetes tend to be hyperreactive. The researchers applied a Piezo1 activator to the blood of people with and without diabetes. In the blood of diabetics, this treatment triggered a five-fold higher percentage of platelets to show signs of platelet activation to a pro-thrombotic state, compared to the blood of non-diabetics.
Using microfluidic devices to mimic the abnormal flow patterns often observed in diabetics’ blood vessels, the researchers tested the clotting behavior of patient blood samples in response to mechanical stress. When a Piezo1 inhibitor was applied, clots were smaller and formed more slowly. Diabetic patients’ blood was more sensitive to the effect of the inhibitor, reinforcing a link between Piezo1 and the clotting propensity seen in diabetes.
Clinical Relevance of Mechanosensation, Hyperglycemia, and Diabetes Link
To investigate the clinical relevance of these findings, the researchers sorted patients with type 2 diabetes into a high-Piezo1 response and a low-Piezo1 response group. Medical records showed that the former group had more macrovascular complications than the latter group (P = 0.04).
This research will help doctors and scientists understand the dysregulated clotting in diabetes and could help researchers develop future therapies or laboratory tests for clotting risk based on Piezo1.
The authors point out that their work could pave the way for future treatment strategies for diabetics that help prevent abnormal clots generated through the mechanothrombotic pathway, potentially presenting less risk of bleeding than current strategies. They also suggest that Piezo1 expression on endothelial cells may be an important part of this picture, though this was not investigated in the study and could be another direction for future research.
Also read
Childhood Diabetes and Sugar Addiction