Understanding irritable bowel syndrome symptoms, causes, diagnosis, management, and emerging research insights. Irritable bowel syndrome is rarely difficult to diagnose. What remains difficult is understanding why the same diagnosis behaves so differently across patients.
In both clinical practice and real-world data, IBS appears less as a single condition and more as a pattern of fluctuating symptoms shaped by gut sensitivity, microbial activity, stress exposure, and individual pain thresholds. This variability explains why standardized treatment pathways often fall short and why IBS continues to challenge clinicians and patients despite its high prevalence.
Real-world survey data reinforces this variability. In a multi-market IBM survey of IBS patients, nearly 90% reported experiencing symptoms frequently or very frequently, yet symptom combinations and perceived triggers differed markedly between individuals.
Rather than asking what IBS is, current thinking increasingly focuses on why symptoms escalate, recede, and re-emerge over time. That shift has important implications for how IBS is interpreted, studied, and managed today.
How IBS Manifests in Daily Life?
What distinguishes IBS in real-world settings is not the presence of symptoms, but their instability. Many patients describe periods of relative control followed by abrupt symptom escalation, often without an identifiable trigger.
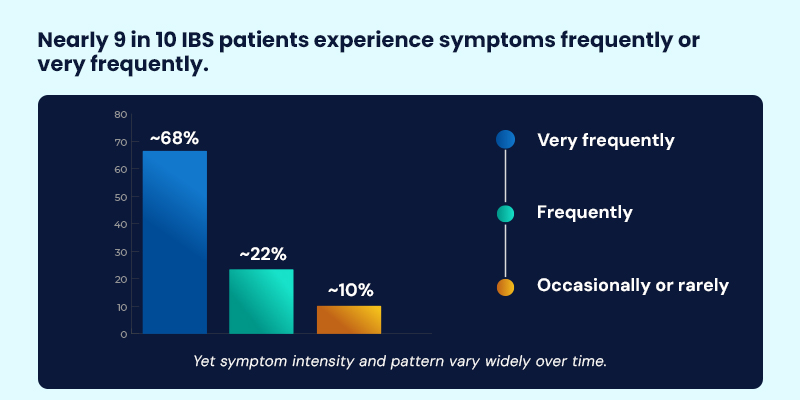
IBM survey findings show that while 68% of respondents experience IBS symptoms very frequently and another 22% frequently, the specific symptom profile often shifts over time—reinforcing the episodic, non-linear nature of IBS.
Commonly reported experiences include recurrent abdominal pain linked to bowel movements, bloating that worsens as the day progresses, diarrhea or constipation or alternating bowel habits, and a persistent sensation of incomplete bowel emptying.
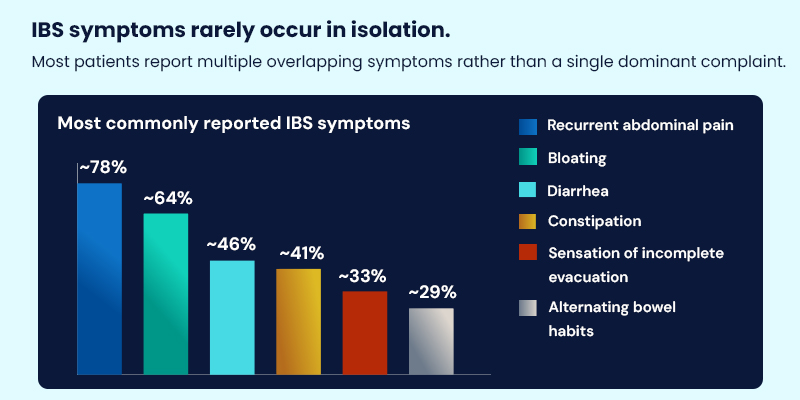
Survey data highlights that IBS symptoms rarely occur in isolation. Approximately 78% of respondents reported recurrent abdominal pain, 64% bloating, 46% diarrhea, and 41% constipation, with many reporting multiple symptoms concurrently rather than a single dominant complaint.
This episodic pattern complicates management and contributes to repeated care-seeking. Insights drawn from patient-reported experiences across platforms such as MDForLives reveal how IBS symptom patterns fluctuate over time, often diverging from what episodic clinical encounters capture about daily functioning, work productivity, and emotional wellbeing.
IBS Subtypes: Useful Categories, Incomplete Explanations
IBS is commonly grouped by predominant bowel patterns such as constipation-predominant, diarrhea-predominant, or mixed forms. These subtypes are helpful for initial clinical orientation and symptom-based treatment decisions.
However, they rarely explain the full picture. Many individuals transition between subtypes over time, and pain severity or quality-of-life impact does not consistently align with bowel habit alone. This reinforces the idea that IBS reflects shifting physiological dynamics rather than fixed diagnostic categories.
Consistent with this, IBM survey responses show that nearly one-third of respondents report alternating bowel habits, and many experience transitions between constipation, diarrhea, and mixed patterns over time—often independent of pain severity.
What Drives IBS Symptoms?
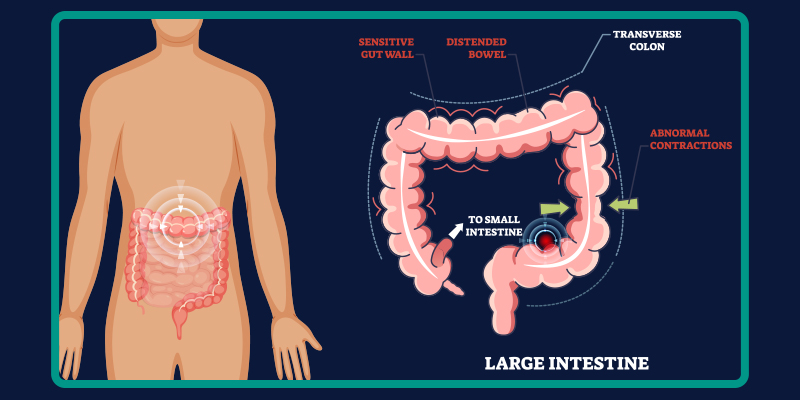
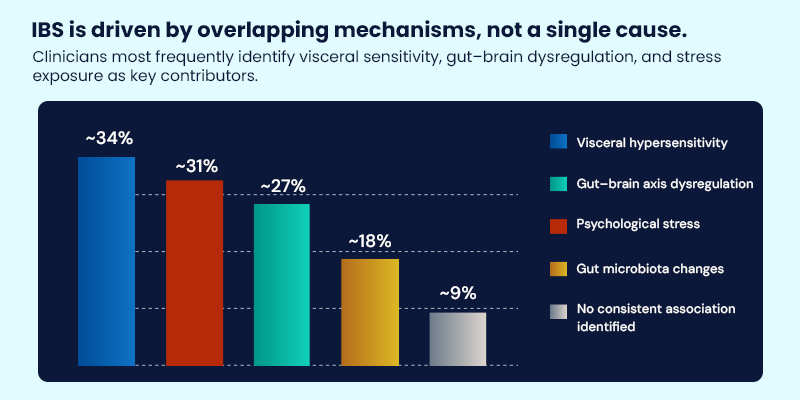
IBS is no longer understood as the result of a single disrupted process. Instead, symptoms emerge from overlapping mechanisms whose influence varies between individuals and across time.
When asked to identify key contributors to IBS symptoms, clinicians most frequently cited visceral hypersensitivity (≈34%), gut–brain axis dysregulation (≈31%), and psychological stress (≈27%), while gut microbiota changes (≈18%) were also commonly noted. Only a small minority reported no consistent underlying association.
Contributing factors include altered gut motility, heightened visceral sensitivity, dysregulated gut–brain communication, post-infectious changes, psychological stress, and differences in gut microbiota composition
Research into the evolving understanding of gut microbes and diet interactions continues to deepen insight into these mechanisms.
Managing IBS in Practice
IBS management is rarely linear. Strategies that appear effective at one stage may lose relevance as symptoms evolve, requiring ongoing adjustment rather than definitive resolution.
Real-world responses reflect this complexity. In the IBM survey, clinicians most often described IBS management as relying on combined or multimodal strategies, rather than single interventions, reflecting the shifting dominance of symptoms and triggers over time.
Eating Patterns
Some individuals experience symptom improvement with changes in fermentable carbohydrate intake, fiber balance, or meal timing. Responses are highly individual and often need periodic reassessment.
Activity and Daily Routine
Regular physical activity has been associated with improved bowel regularity and stress modulation, particularly in individuals whose symptoms worsen during periods of psychological strain.
Psychological and Behavioral Approaches
Because IBS symptoms are closely linked to pain perception and stress response, therapies addressing the gut–brain axis may play a meaningful role for selected patients.
Medications
Pharmacological options are used to target specific symptom clusters such as bowel habit irregularity or heightened pain sensitivity, typically as part of a broader management approach.
Who Is More Likely to Develop IBS?
Population-level observations suggest that IBS does not arise randomly. Certain factors appear more frequently among those diagnosed, including female sex, family history of functional bowel disorders, prior gastrointestinal infections, chronic stress, and alterations in gut microbiota composition.
These patterns highlight how biological vulnerability and live experience intersect rather than pointing to a single causal pathway.
Diagnosing IBS: Pattern Recognition Over Proof
Diagnosing IBS is less about confirming a disease and more about recognizing consistent symptom patterns while excluding alternative explanations. Clinical assessment and symptom-based criteria guide diagnosis rather than reliance on definitive laboratory findings.
Survey findings support this approach: clinicians emphasized symptom pattern recognition and longitudinal assessment over isolated test results, noting that symptom persistence and variability were more informative than any single diagnostic marker.
This approach reflects the functional nature of IBS and helps differentiate it from overlapping bowel conditions, including chronic constipation and other gastrointestinal disorders.
Testing: What Is and Is Not Routine
Laboratory Testing
Blood and stool tests may be used selectively to rule out inflammation, infection, or metabolic conditions when clinically indicated.
Imaging and Endoscopy
Imaging and endoscopic evaluations are not routine for IBS and are generally reserved for cases with alarm features such as unexplained weight loss or gastrointestinal bleeding.
Can IBS Be Prevented?
There is no established method to prevent IBS entirely. However, early management of gastrointestinal infections, attention to stress, and maintaining regular eating and activity patterns may reduce symptom persistence or severity in some individuals.
Emerging Research: Rethinking IBS Pain
Recent IBS research has shifted focus from defining the condition to understanding why pain intensifies in certain patients. One emerging area of interest involves microbiome-mediated pathways that influence immune activation and pain signaling.
Studies have identified Klebsiella aerogenes as a high histamine-producing gut bacterium in a subset of IBS patients. Elevated histamine levels have been associated with mast cell activation and increased visceral hypersensitivity, offering a biological explanation for pain flares that occur independently of bowel habit changes.
Real-world survey data echoes this dissociation between pain and bowel habits. Many respondents reporting severe or frequent abdominal pain did so without consistent alignment to constipation or diarrhea patterns, supporting emerging models of microbiome- and immune-mediated pain amplification.
Dietary modulation appeared to influence this pathway, with reduced fermentable carbohydrate intake associated with lower histamine levels and reduced pain sensitivity. While these findings apply only to a subset of patients, they support the growing view of IBS as a condition defined by mechanistic subgroups rather than a single disease model.
Interpreting IBS research increasingly requires integrating clinical findings with longitudinal patient-reported data. Platforms such as MDForLives help surface real-world symptom variability and trigger patterns that are difficult to observe within controlled trial settings alone.
Conclusion: Why IBS Understanding Is Shifting
What real-world data adds to IBS research is context. Survey insights reveal where symptoms fluctuate unpredictably, where mechanisms overlap rather than dominate, and where
standardized pathways fail to reflect lived experience. By capturing longitudinal, patient- and clinician-reported patterns, platforms such as MDForLives help shift IBS understanding from rigid categories toward dynamic, mechanism-informed care.
Frequently Asked Questions
Is irritable bowel syndrome (IBS) a lifelong condition?
Irritable bowel syndrome is a chronic condition, but symptoms are not constant. Most people experience fluctuating periods of symptom flare and remission rather than continuous discomfort. IBS often changes in severity and presentation over time, influenced by gut sensitivity, stress exposure, and individual pain response rather than progressive disease.
Why do IBS symptoms flare without an obvious trigger?
IBS symptoms can flare due to changes in gut–brain signaling, visceral hypersensitivity, immune activation, or gut microbiota activity, even when diet and routine remain unchanged. Emerging research shows that pain pathways in the gut may amplify independently of bowel habits, explaining why flares sometimes occur without clear external triggers.
Why is there no definitive test for diagnosing IBS?
There is no single diagnostic test for IBS because it is a functional gastrointestinal disorder, not a structural disease. Diagnosis is based on consistent symptom patterns and clinical evaluation, with laboratory or imaging tests used selectively to rule out other conditions when warning signs are present.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.