New research shows the global prevalence of obesity and its contribution to the pathogenesis of polycystic ovary syndrome (PCOS). Barber and Franks explored the effects of obesity on the pathogenesis of PCOS from the perspective of each of the main features of the disease that are metabolic dysfunction, hyperandrogenism, and reproductive dysfunction, and described in the August 2021 publication. The lifestyle strategies that should be considered for the long-term management of PCOS in obese women are also described in the same publication.

What is PCOS?
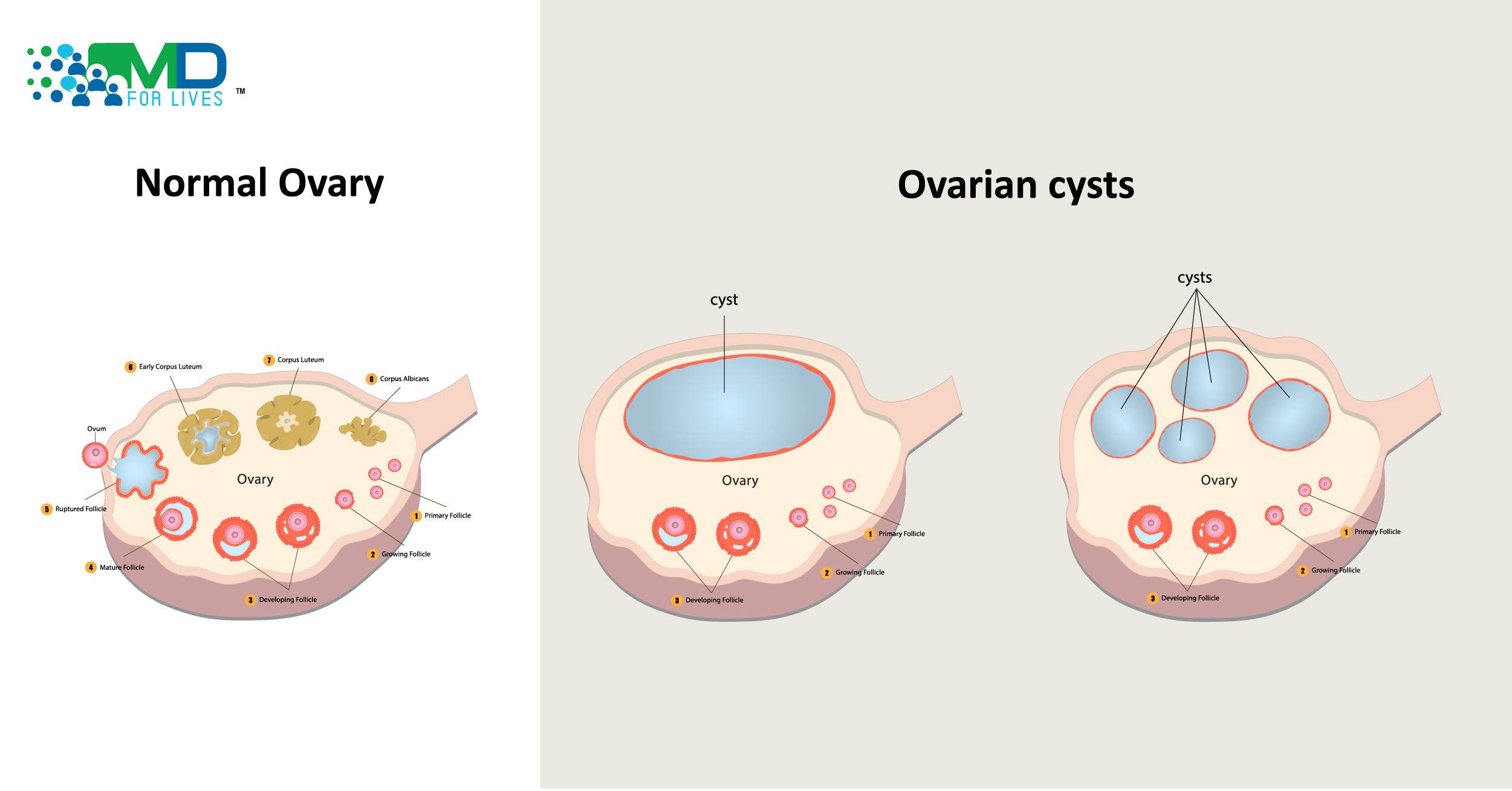
PCOS is a disorder of the female reproductive system that manifests metabolic disturbances such as obesity, insulin resistance, and diabetes mellitus. PCOS increases the risk of developing Type 2 diabetes and cardiovascular disease. Elevated androgen levels, menstrual irregularities, and/or small cysts on one or both ovaries are generally observed in PCOS women. Elevated androgen levels lead to hirsutism, acne, and alopecia. PCOS affects 5% to 10% of females between the ages of 18 and 44. It is fairly common to have a family history of PCOS. PCOS is caused by primary defects in the hypothalamic–pituitary axis, insulin secretion and action, and ovarian function. Follicular maturation arrest in PCOS women indicates the abnormality of the ovary. Luteinizing hormone (LH) and gonadotropin-releasing hormone (GnRH) levels increase and levels of the follicular-stimulating hormone (FSH) get muted or remain unchanged. Increased GnRH levels lead to the production of more androgens.
As an Obstetrician-Gynecologist, your role extends far beyond the clinic. Participate in paid Ob gyn surveys with MDForLives, share your insights
 Symptoms of PCOS
Symptoms of PCOS
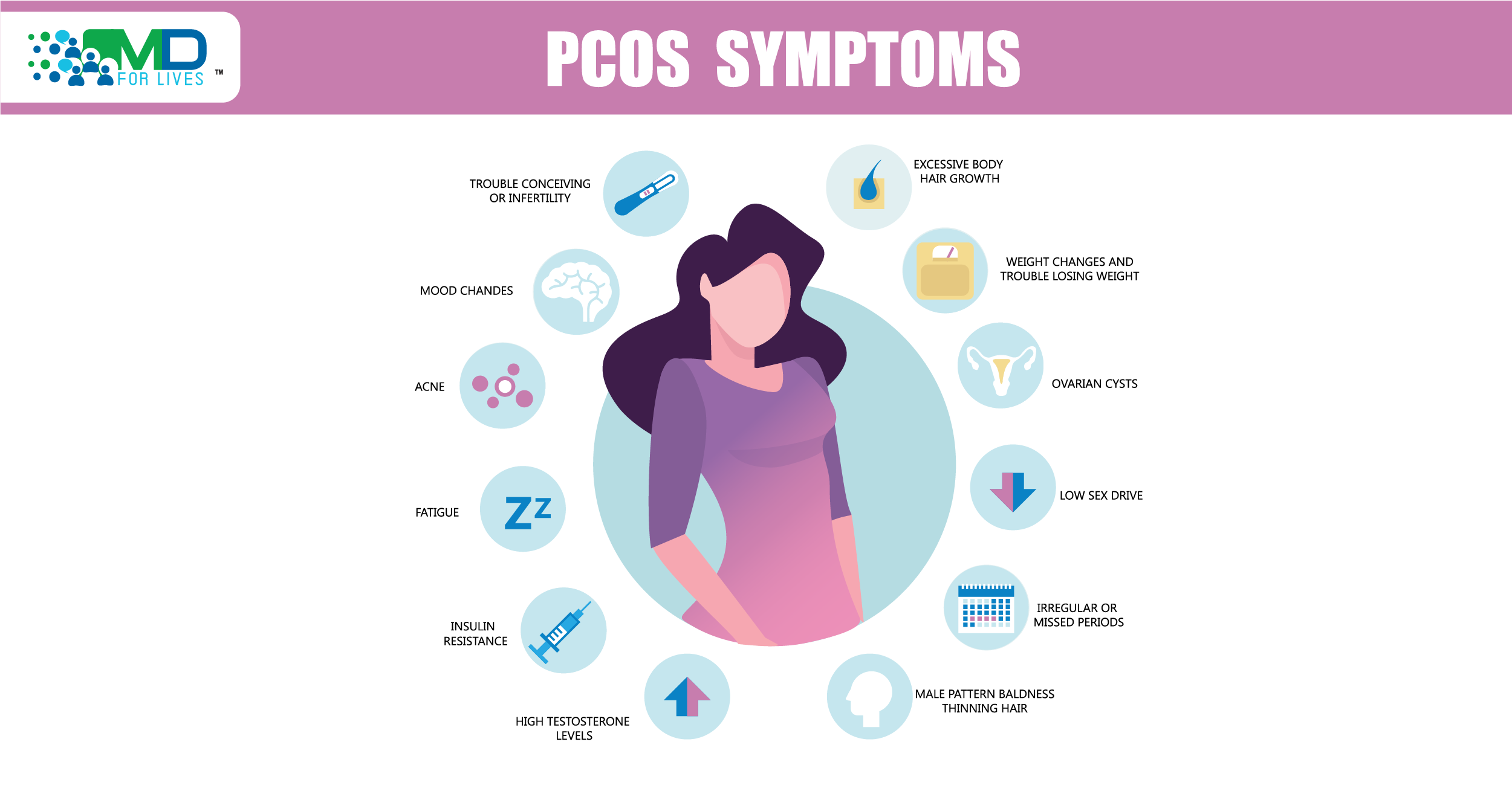
Irregular menstrual cycles are the main symptom of PCOS; in fact, PCOS is the cause of pelvic pain, hirsutism, alopecia, acne, skin tags, low sex drive and fatigue in many women. Defects in the maturation of the hypothalamic-hypopituitary-ovarian axis lead to menstrual irregularities. Due to endocrine and gynecologic abnormalities that affect ovarian quality and function, women with PCOS may have lower fertility.
 Treatment of PCOS
Treatment of PCOS
Treatment of polycystic ovary depends on the symptoms of the patient and also the need to get pregnant. Weight loss is advised for patients who are overweight. Clomiphene and letrozole are first-line infertility medications. Metformin is the first-line treatment for metabolic symptoms such as hyperglycemia. Hormonal contraception is the first-line treatment for irregular menstruation and dermatological manifestations. Aromatase inhibitors, letrozole, are linked to higher rates of live birth and ovulation in infertile women with polycystic ovary syndrome. Letrozole affects hypothalamic–pituitary–ovarian function and thereby increases pregnancy rates. Metformin improves insulin action as well as anovulation. For clinical manifestations of PCOS, such as menstrual irregularity, hirsutism, and acne, combined hormonal contraceptives are the first-line management options. These alleviate hyperandrogenism symptoms by lowering androgen production.

 Research uncovers the contribution of obesity in the pathogenesis of polycystic ovary syndrome
Research uncovers the contribution of obesity in the pathogenesis of polycystic ovary syndrome
PCOS is a significant and widespread obesity-related comorbidity. Obesity is observed between 38% and 88% of women with PCOS. There is a shared genetic architecture between obesity, various metabolic traits and PCOS. The defect in the mechanism of insulin resistance in PCOS is thought to occur in the post-receptor phosphatidylinositol 3-kinase (PI3-K) insulin pathway, which mediates insulin’s metabolic effects. Increased plasma testosterone levels, enhanced androgen receptor sensitivity and reduced serum adiponectin levels also contribute towards the establishment of insulin resistance. Following weight gain, the PI3-K post-receptor insulin pathway becomes insulin resistant and worsens the severity of insulin resistance in women with PCOS.


Adipokine levels in serum are typically associated with body fat mass and the severity of obesity. Many adipokines have an impact on insulin sensitivity as well as overall cardiometabolic risk. Serum levels of visfatin, one of the adipokine, are higher in women with PCOS and this elevated level of serum visfatin in PCOS may therefore contribute towards insulin resistance and metabolic dysfunction.
Women with PCOS have a 2-fold higher risk of developing obstructive sleep apnoea, which occurs due to the typical hormonal changes of PCOS. In women with PCOS, visceral fat content increases the risk of obstructive sleep apnoea.


Increased amounts of visceral and hepatic fat contribute to PCOS. Obese women with PCOS are more likely to develop non-alcoholic fatty liver disease (NAFLD), due to hepatic fat. Overall weight gain and obesity linked to the visceral fat volume are likely to contribute to insulin resistance and metabolic dysfunction in PCOS. Weight gain contributes to hyperandrogenaemia in PCOS women.
Weight Loss and PCOS – Effective Management
Consumption of low calorie and weight loss reduces hyperinsulinaemia while improving the hyperandrogenic and reproductive features of PCOS.


Physical activity boosts insulin sensitivity and reduces overall cardiovascular risk. As an effective means of weight loss through lifestyle change, physical activity frequently complements dietary changes. PCOS patients should engage in regular physical activity for 30-60 minutes per day, but should not overdo it. For overall health and wellbeing and achieving weight loss, the dietary modification should be recommended. Monounsaturated fat-enriched and low-carbohydrate diets correspond to greater weight loss and improved menstrual regularity. A high-protein diet is linked to less depression and higher self-esteem.


The success of implemented weight-loss lifestyle measures appears to be dependent on a prerequisite of adequate sleep. Sleep sufficiency is highly important in women with PCOS, and to get a proper amount of sleep, avoidance of blue light from screens during the late evening, cooling the body prior to sleep and avoidance of food and exercise before sleep are recommended. Mindfulness is a state of being that allows for heightened awareness of one’s own internal emotions as well as one’s immediate surroundings. Mindfulness can be beneficial to the clinical management of PCOS.
Also read
National Women Health and Fitness Day
Gender Based Pay Gaps in Healthcare