Have you noticed people reaching out for antibiotics at the first sign of a cold, or change in weather? This casual misuse is feeding a silent, escalating threat – Antimicrobial Resistance (AMR). Once easily treated, infections are becoming harder to cure, and this isn’t a distant problem; it’s happening right now. Recent studies show that by 2025, AMR could be responsible for 39 million deaths, overtaking cancer as a leading cause of mortality. AMR occurs when bacteria, viruses, and other microbes evolve to resist the drugs meant to kill them, rendering treatments ineffective and increasing the risk of severe illness or death.
In this growing crisis, pharmacists are emerging as crucial defenders on the frontlines. Their expertise in medication management, public education, and antibiotic stewardship positions them uniquely in the fight against the threat of antimicrobial resistance. In this blog, we explore the indispensable role pharmacists play in countering AMR and why their involvement is more critical now than ever.
Threat of Antimicrobial Resistance – Key Factors
There are several key factors that contribute to the growing problem of antimicrobial resistance. These include both human behaviors and systemic issues that accelerate the ability of microbes to resist treatment.
Some of the most common contributing factors are:
- Antibiotic Overuse: Every unnecessary dose and misuse of antimicrobial drugs chips away at their effectiveness, empowering bacteria to evolve and fight back. The more frequently they are used without cause, especially in farming and minor infections, the faster resistance spreads.
- Antibiotic Misuse: Took antibiotics for your last cold? It probably didn’t help, as cough and cold are usually caused by viruses, not bacteria. But beyond being ineffective, such misuse contributes to the threat of antibiotic resistance.
Each unnecessary dose gives bacteria more opportunity to adapt, making it harder to treat infections in the future. - Incompletion of the Antibiotic Course: When patients stop taking antibiotics midway, they leave behind surviving bacteria that can adapt and become resistant. This incomplete treatment fuels the growing threat of antimicrobial resistance. So, when you stick to the full course, you are not just healing yourself but helping prevent the next wave of superbugs.
What’s Fueling the Global AMR Surge in 2025?
Do you often wonder how we got into this storm of AMR crisis? The rise of superbugs is not happening by chance. There are several factors that contribute to the increase in antimicrobial resistance:
1. The DIY self medication issues
In many countries, antibiotics are available without any prescription. It is offered over the counter by pharmacists in an unregulated manner. So, your friendly neighbor, James, will pop in amoxicillin whenever he feels under the weather. He will also decide how much to take and the course as well!
Such DIY issues roll out the red carpet for bacteria to thrive.
2. When clean isn’t clean enough
Inadequate hygiene practices in hospitals and communities deepen the spread of resistant pathogens. For example, hospital-acquired infections caused by drug-resistant bacteria like MRSA are increasingly common. They can travel from room to room on unwashed hands or improperly sterilized medical equipment.
3. Agricultural use
Antibiotics are widely used in livestock farming to promote growth and prevent diseases. This contributed significantly to emerging antibiotic resistance. This is because these strains can transfer to humans from animals through food or direct contact with humans. When they transfer from livestock to humans, they bring their antibiotic resistance along for the ride.
Threat of Antimicrobial Resistance – How Pharmacists Help Tackle?

When we think of frontline heroes battling deadly bacterial infections, our minds often go first to physicians working tirelessly in hospital wards. However, there is another group of essential fighters in this battle – those found in both community and hospital pharmacies.
Pharmacists, as medication experts, play a pivotal role in the fight against the threat of antimicrobial resistance. They serve not only as healthcare providers but also as leaders, educators, and implementers of strategies that help curb the spread of resistant infections.
Let us see how they fight against the AMR terror:
1. They Double-Check Prescriptions
Ever wondered why your pharmacist steps away with your prescription? It is not just about counting pills or calculating costs. Behind the counter, they are carefully reviewing whether the antibiotic prescribed is right for you. They delve into factors like – your condition, age, existing medications, allergies, and even dosage availability.
They also assess if a more targeted antibiotic could be used instead of a broad-spectrum one. If something seems off, they do not hesitate to contact the prescribing doctor. This crucial intervention helps prevent unnecessary antibiotic use and is one of the most effective frontline defenses against the rising threat of antimicrobial resistance.
2. They Are the Ultimate “Myth-Busters”
“But I always take Azithromycin for my sinus colds!”
Pharmacists hear this all the time and have become master educators in response. They apply patience and use accessible language to explain why antibiotics cannot work in case of viral infections like the common cold or many cases of bronchial infections.
Also, they can dispel misconceptions about antibiotics being a cure-all for infections.
Some of the common myths include:
- Explaining that antibiotics do not work against viral infections like colds or flu.
- Highlighting risks associated with misuse, such as increased hospitalizations due to resistant infections.
These educational moments happen several times across thousands of pharmacies all over the world. The result is that it helps gradually shift public understanding about appropriate antibiotic use.
3. They Support Antibiotic Stewardship Programs
In hospitals, pharmacists are on the frontline of antimicrobial stewardship; not to restrict antibiotics, but to protect them. They evaluate prescriptions, monitor resistance trends, and collaborate with physicians to ensure the right drug, dose, and duration.
From switching IV to oral meds to narrowing therapy, pharmacists’ decisions curb resistance, cut costs, and improve recovery.
4. They Monitor, Report, and Respond.
Pharmacists often spot what individual prescribers might overlook. They track antibiotic dispensing trends across multiple sources, giving them a broader view of prescribing behaviors. A sudden spike in demand for a specific antibiotic at a local pharmacy, for instance, could signal an outbreak or the early signs of emerging resistance.
Acting as sentinels in our antimicrobial defense system, pharmacists play a critical role in identifying and reporting unusual patterns in disease progression. Their vigilance helps detect brewing threats before they escalate.
5. They Act as Healthcare Team’s Intermediary
In today’s world, healthcare achieves the best outcomes through collaborative teamwork. Pharmacists play a vital role in uniting doctors, nurses, and patients because of their involvement with antibiotics. Their knowledge of drugs, in addition to the physician’s diagnosis, is an amazing combination. They form a strong team that fights against the misuse of such drugs as antibiotics.
If a pharmacist proposes a different medication or questions a prescription, they do not question the doctor’s authority. Instead, this act seeks to add value through specialized knowledge that is necessary for ensuring the safety of the patient and the proper use of available antibiotics.
This reflects the pharmacist’s roles and responsibilities in managing global antimicrobial resistance.
6. They Serve as Medication Mentors
Pharmacists also help patients with complex medication regimens. They provide effective medication therapy management services that go far beyond simply dispensing pills. They take time to explain why finishing an entire antibiotic course is critical, even when symptoms improve.
Additionally, they help patients understand possible side effects and interactions. Doing so increases the likelihood that treatments will be completed as prescribed.
These personalized consultations build trust and improve adherence. They turn out to be crucial elements in preventing the development of resistant infections.
Hospital vs Community Pharmacists: Distinct Roles, Unified Purpose!
It is true that all pharmacists fight against the threat of antimicrobial resistance. However, their battlegrounds differ a lot. Community pharmacists serve on the public frontlines. On the other hand, hospital pharmacists work behind the scenes in clinical settings. Though their environments and daily responsibilities vary, both play equally crucial roles in preserving antibiotic effectiveness.
Let’s take a closer look at how these two roles complement each other in the ongoing battle against AMR.
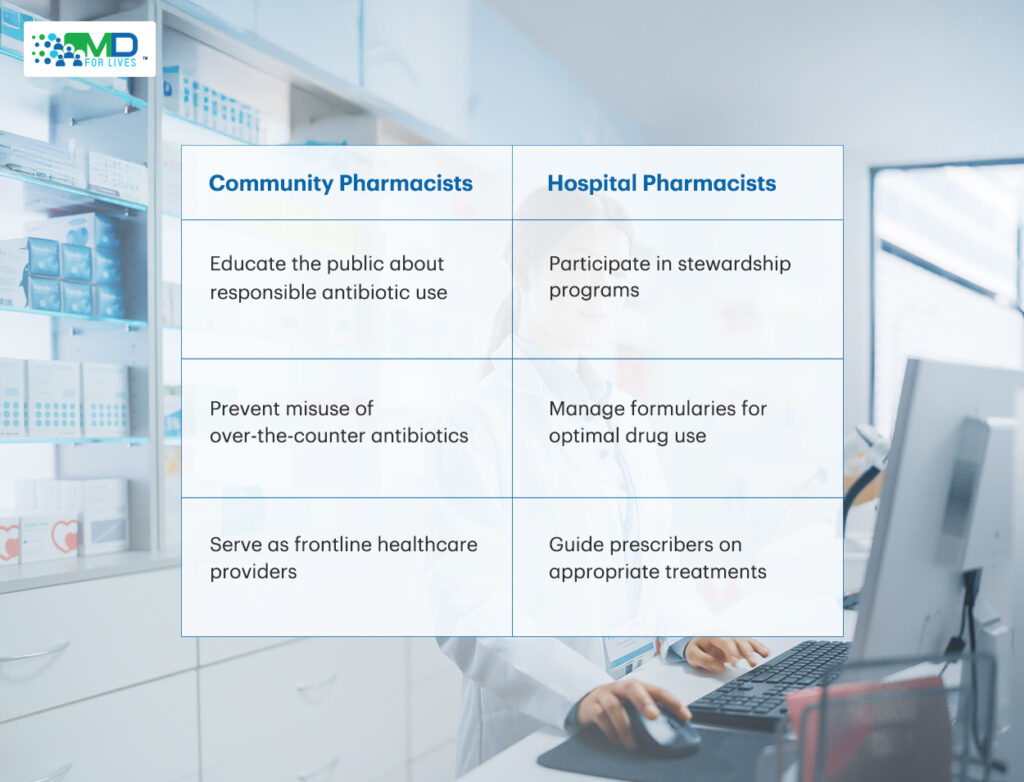
Community pharmacists are usually the first point of contact for patients seeking medication advice. They play a key role in preventing self-medication and promoting awareness about emerging antibiotic resistance among the public.
Hospital pharmacists work closely with physicians as part of multidisciplinary teams focused on antimicrobial stewardship efforts. Their responsibilities include managing formularies and monitoring drug usage patterns. They also adhere to prescribing guidelines, highlighting the role of pharmacists in managing increasing antibiotic resistance.
Barriers Pharmacists Encounter in Combating Antimicrobial Resistance
Pharmacists encounter a lot of challenges despite their critical role. Some of the challenges are mentioned below:
1. Pressure to Dispense Antibiotics
Patients often demand unnecessary antibiotics, and this raises the threat of antimicrobial resistance. This is mainly due to misconceptions about their effectiveness against viral infections like cold or flu.
2. Limited Access to Patient Records
In many settings, pharmacists lack access to patient records that are needed for informed decision-making regarding prescriptions.
3. Insufficient Training on AMR
In some areas, pharmacists lack knowledge about global antimicrobial resistance trends. This is mainly due to limited training opportunities. This can be another challenge that impedes the efficacy of a pharmacist in tackling the menace of AMR.
4. Public Misconceptions
Many people mistakenly believe that antibiotics are effective against all types of infections. This is a misconception that fuels inappropriate demand for these drugs.
What Steps Can Strengthen Pharmacists’ Role in Tackling AMR?
If pharmacists are our frontline defenders against the threat of antimicrobial resistance, then we need to make sure they are equipped with the right tools and knowledge. Several strategic initiatives must be implemented across healthcare systems worldwide to strengthen pharmacists’ role in combating AMR effectively.
1. Continuous education so that they never stop learning
Remember how quickly science class information became outdated after you left school? The world of microbiology and antimicrobial therapy moves even faster!
Today’s pharmacy graduates need more than their degrees hanging on the wall. They need ongoing education that keeps pace with evolving resistance patterns. It will not be feasible for a pharmacist who graduated ten years ago to try to combat today’s superbugs with a decade-old knowledge. It simply won’t work.
Regular training programs on increasing antibiotic resistance trends should be mandatory for all practicing pharmacists. These educational initiatives must go beyond basic awareness to include detailed microbiology updates and therapeutic alternatives to commonly overused antibiotics.
Pharmacists require exposure to expert courses that boost their clinical decision-making skills in the area of antimicrobial therapy. Such training should be based on case studies that mirror actual real-life situations pharma professionals deal with on a day-to-day basis.
Some forward-thinking professional organizations are creating “AMR Specialists” through advanced certification programs. These pharmacists become the local experts who can guide their colleagues through particularly thorny resistance challenges. It is just like having an antimicrobial resistance coach on the speed dial.
2. Regulatory frameworks for strict implementation of rules
Good intentions are just not sufficient when it comes to preserving antibiotic effectiveness. We need rules with consequences. Governments must implement policies that restrict indiscriminate dispensing practices while ensuring those with legitimate needs get access to treatment.
These frameworks should include:
- Prohibiting the sales of antibiotics without proper prescriptions.
- Mandating a pharmacist’s verification of prescriptions.
- Establishing penalties for non-compliance with AMR-related regulations.
And let’s not forget the shadowy world of counterfeit antibiotics. These pills may contain little or no actual medication but contribute enormously to resistance by exposing bacteria to subtherapeutic doses.
Regulatory frameworks must tackle this underground market that undermines legitimate healthcare.
3. Strategies that help pharmacists work in sync with healthcare experts
Pharmacists should be integrated into multidisciplinary teams alongside infectious disease physicians and public health officials. Their contributions can include:
- Developing local prescribing guidelines based on resistance patterns.
- Participating in Antimicrobial Stewardship Programs or ASPs to optimize antibiotic use in hospitals and ambulatory care settings.
- Providing feedback to prescribers regarding inappropriate antibiotic choices.
Even in community settings, pharmacists and primary care providers can develop collaborative relationships against the threat of antimicrobial resistance. When this happens, patients benefit from more appropriate antibiotic prescribing. That urgent care provider might think twice about prescribing azithromycin for a viral infection if they know the local pharmacist will be calling to discuss alternatives.
4. Spreading the word for community education on ‘AMR’
Facts alone can rarely change behavior; but good storytelling can!
Pharmacists are perfectly positioned to lead community education efforts that transform how the public thinks about antibiotics. Through creative campaigns that speak in everyday language, pharmacists can:
- Promoting hand hygiene and infection control practices.
- Dispelling myths about antibiotics being a cure-all for infections.
- Encouraging vaccinations to prevent bacterial infections.
When a trusted local pharmacist explains, using real-life stories, why antibiotics aren’t needed for something like a common cold, the message resonates more deeply than standard clinical warnings. These personal, relatable conversations help shift public perception and promote responsible antibiotic use. Social media platforms and community outreach programs can enhance this impact. Campaigns such as Antibiotic Awareness Week have successfully engaged communities worldwide, building greater understanding of the risks associated with antimicrobial resistance (AMR).
Supercharging Pharmacists: The Fight Against AMR Begins Here!
The war against the threat of antimicrobial resistance isn’t confined to doctors or hospitals alone. It’s unfolding quietly across local communities, where pharmacists play a crucial role. Often the first point of contact for patients, pharmacists act as vigilant gatekeepers educating the public, promoting the responsible use of antibiotics, and guiding better healthcare decisions that safeguard both present and future generations.
But let’s be honest; they can’t fight this battle alone. To create real, lasting impact, pharmacists need stronger policies, public awareness, and robust support from the healthcare ecosystem.
The time to act is NOW.
If you’re a pharmacist, your voice matters. Join MDForLives, a community of allied healthcare professionals helping shape the future of medicine. Participate in paid medical surveys, contribute to real-world research, and be a part of the global solution to the AMR crisis.
FAQs
What exactly is antimicrobial resistance (AMR)?
Antimicrobial resistance happens when microbes become resistant to drugs. Infections become more difficult to treat. Misuse and excessive use of antimicrobials are the biggest causes of this worldwide health risk.
How can pharmacists help reduce AMR?
Pharmacists play a key part in antimicrobial stewardship. They optimize antibiotic use and educate patients. They also promote adherence to guidelines and advocate responsible prescribing practices to curb resistance.
Why is antibiotic misuse such a big problem?
Antibiotic misuse accelerates resistance. This leads to ineffective treatments and prolonged illnesses. It also results in higher healthcare costs and increased mortality risks.
Can pharmacists refuse to dispense antibiotics if misused?
Pharmacists can legally refuse prescriptions suspected of misuse, depending on state laws. They must provide clear explanations or referrals in some jurisdictions while prioritising patient safety.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.






