Epilepsy, a neurological condition marked by recurrent seizures, poses distinct challenges for both patients and healthcare providers. Recent studies have brought attention to the complex connection between sleep and seizures, especially in individuals with sleep-related epilepsy. Sleep is pivotal in regulating neuronal excitability and synchronization, affecting seizure threshold and susceptibility. In sleep-related epilepsy, seizures frequently follow circadian patterns, with heightened occurrence during particular sleep stages. This emphasizes the importance of delving deeper into the intricacies of sleep architecture and its influence on seizure activity.

As we commemorate International Epilepsy Day, physicians need to raise awareness about the multifaceted nature of epilepsy and its impact on individuals worldwide. This global initiative aims to increase understanding and support for those affected by epilepsy, highlighting the need for continued research, education and advocacy efforts. By shedding light on the relationship between sleep and epilepsy, we can contribute to improving the lives of individuals living with epilepsy and advancing the field of epilepsy care on a global scale.
To fully grasp how sleep and epilepsy are connected and to learn about the strategies physicians can use to deal with sleep-related epilepsy, keep reading.
THE DYNAMIC RELATIONSHIP BETWEEN SLEEP AND SEIZURES
Before exploring the intricate connection between sleep and epilepsy/seizures, it’s essential for every physician to understand this fundamental fact:
As per the ‘Sleep Foundation,’ approximately 15% of individuals with epilepsy experience seizures exclusively during sleep or shortly after waking up.
Sleep and epilepsy share a bidirectional relationship, where disruptions in sleep patterns can trigger seizures and seizure activity can disrupt sleep architecture. Understanding this interplay is essential for devising comprehensive treatment plans.
- Sleep-Wake Cycle and Seizure Susceptibility: The circadian rhythm influences seizure susceptibility, with certain types of epilepsy exhibiting a preference for specific times of day or night. Nocturnal seizures, for instance, are prevalent in certain types of epilepsy, highlighting the importance of sleep assessment in epilepsy management.
- Sleep Architecture and Seizure Generation: The various stages of sleep, such as REM (rapid eye movement) and non-REM sleep, impact the seizure threshold differently.
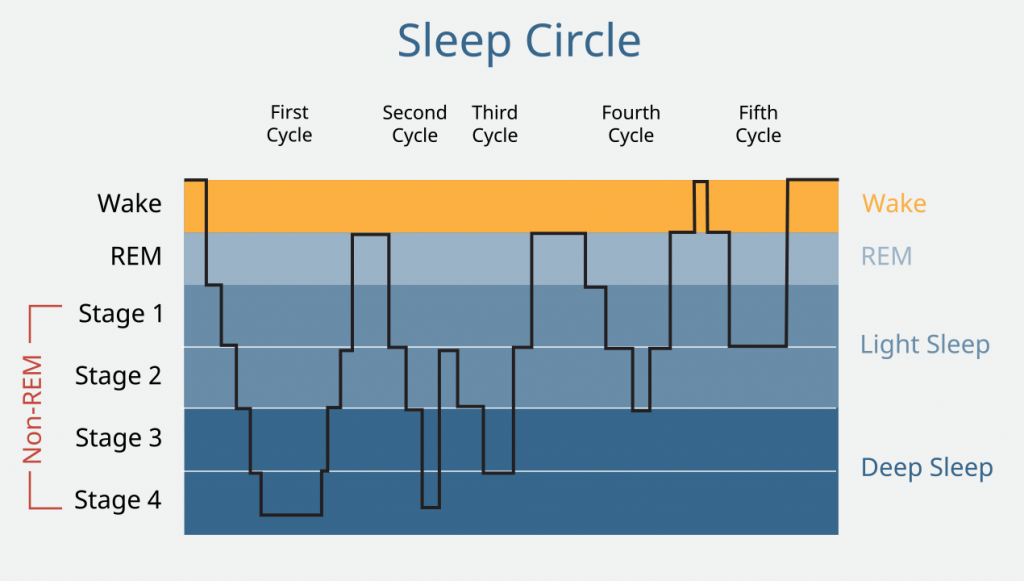
REM sleep, characterized by increased neuronal activity, may lower seizure thresholds, whereas non-REM sleep typically shows higher seizure thresholds. Understanding these nuances can aid in optimizing seizure control strategies.
- Sleep Disorders and Epilepsy: Comorbid sleep disorders, such as obstructive sleep apnea, insomnia and restless legs syndrome, are prevalent among individuals with epilepsy. Addressing these coexisting conditions is paramount, as untreated sleep disorders can exacerbate sleep deprivation seizures frequency and severity.
SLEEP-RELATED EPILEPSY: LISTING OUT THE BEST STRATEGIES FOR PHYSICIANS
Dealing with patients having sleep-related epilepsy requires a multifaceted approach tailored to individual patient needs. Here are a few critical strategies for physicians to optimize epilepsy management in the context of sleep:
- Comprehensive Sleep Assessment: Incorporate thorough sleep evaluation into routine epilepsy assessments, including sleep history, sleep diaries and validated sleep questionnaires. Identifying sleep disturbances early enables targeted interventions to improve seizure control.
- Promotion of Healthy Sleep Hygiene: Educate patients on the importance of maintaining regular sleep-wake schedules, creating a conducive sleep environment and adopting relaxation techniques to enhance sleep quality. Lifestyle modifications such as limiting caffeine and electronic device usage before bedtime can also mitigate sleep disruptions and sleep deprivation seizures.
- Optimization of Antiepileptic Medications: Consider the impact of antiepileptic medications on sleep architecture and vice versa. Tailor medication regimens to minimize sleep disturbances while effectively managing sleep deprivation seizure activity. Collaborate closely with sleep specialists when necessary to optimize pharmacotherapy.
- Treatment of Coexisting Sleep Disorders: Address comorbid sleep disorders through a multidisciplinary approach involving neurologists, sleep medicine specialists and other healthcare professionals. Continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea, cognitive-behavioral therapy for insomnia and pharmacotherapy for other sleep disorders can significantly improve sleep deprivation seizures outcomes.

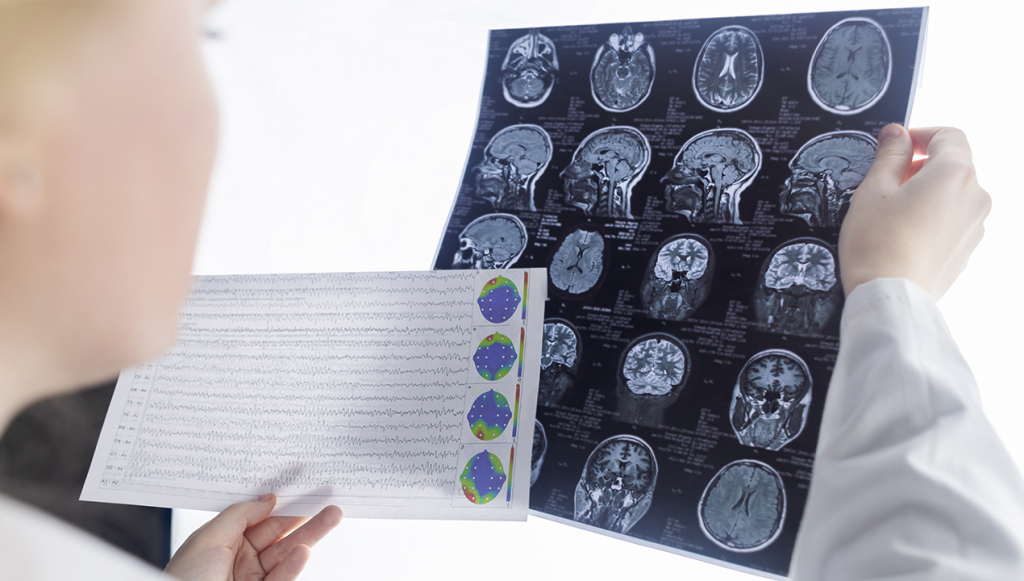
Additional Suggestion: In diagnosing sleep-related epilepsy, employing advanced monitoring techniques like polysomnography and video EEG monitoring is essential. These methods allow physicians to capture real-time data on brain activity and sleep patterns, identifying subtle abnormalities and customizing treatment plans.
CONCLUSION

To sum it all up, it’s pretty straightforward – grasping the connection between sleep and seizures is absolutely crucial when dealing with sleep-related epilepsy. By digging into each patient’s sleep habits and finding treatments that fit them like a glove, we can truly make strides in managing their seizures and boosting their overall well-being.
Let’s stay committed to this holistic approach, tailoring care to fit each individual and keep making a positive impact on their lives.
Discover a whole new avenue for sharing your expertise with MDForLives. By participating in paid medical surveys and contributing insightful articles, you not only amplify your voice but also gain access to exclusive webinars and stimulating discussion forums.
References:
- Sleep and Epilepsy: A Complex Interplay
www.ncbi.nlm.nih.gov - Managing sleep disorders in people with epilepsy
www.sciencedirect.com - The relationship between sleep quality and the severity of insomnia with the frequency of seizures in epileptic patients
www.elsevier.es - Deviations from normal sleep duration and quality can greatly influence the risk of a seizure
www.thelancet.com - Epilepsy and Sleep: Understanding the Relationship
www.sleepfoundation.org

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.



