Pharmacists occupy a critical frontline role in healthcare. They are often the final checkpoint before a patient receives medication, ensuring every prescription is accurate, safe, and personalized. Yet, despite this pivotal responsibility, incomplete prescription or prescription errors remain an “all-too-frequent” reality in pharmacies across the globe.
A recent survey by MDForLives, gathering insights from pharmacists in the UK, Canada, Italy, and Germany, has highlighted a disturbing trend. Incomplete or erroneous prescriptions are no longer a rare mishap; they are a persistent, everyday challenge. These errors are far from trivial. From wrong dosages and illegible handwriting to missing patient information, the potential consequences are profound, directly affecting patient safety, adherence, and treatment outcomes. Pharmacists navigate this high-stakes environment daily, intercepting prescription errors in pharmacy, clarifying instructions, and safeguarding lives, often under immense pressure.
Understanding the frequency and nature of these prescription errors is crucial. That is precisely why MDForLives recently ran a survey to shed light on the most encountered mishaps, the regions where they are most prevalent, and the strategies pharmacists employ to mitigate risk.
Incomplete Prescription: A Daily Struggle for Pharmacists
In the current year, 2025, incomplete prescriptions are not a rare occurrence. According to our survey, pharmacists encounter incomplete medical prescriptions on a regular basis – some daily, others weekly or occasionally, highlighting how widespread the issue has become.
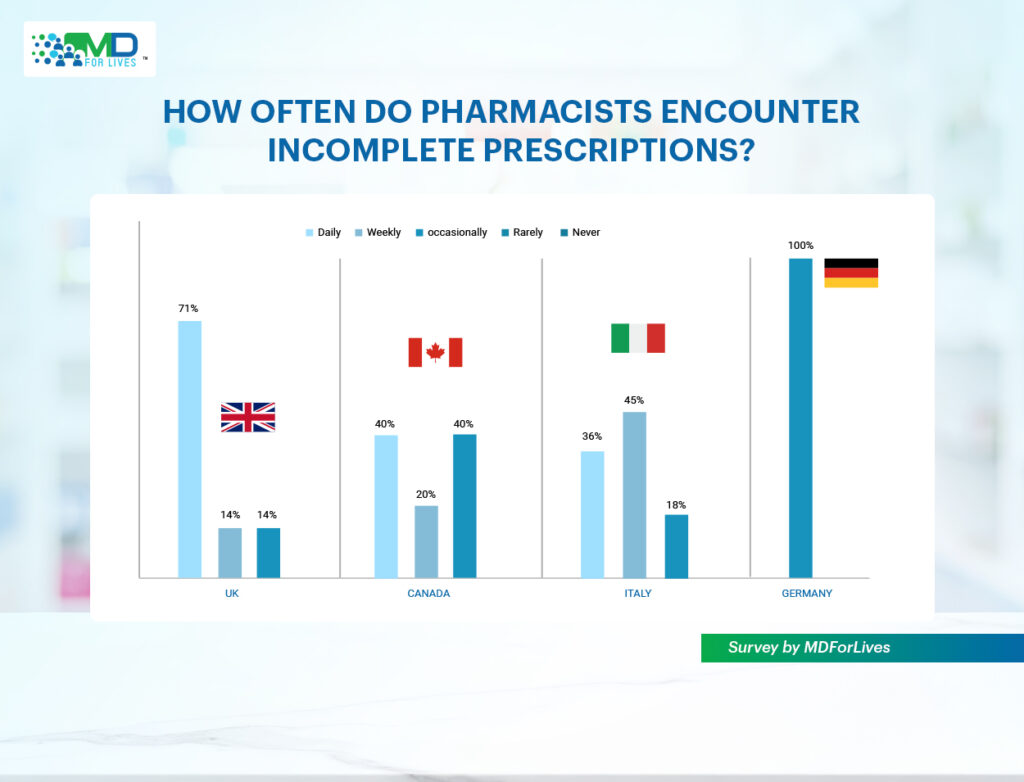
The situation appears most pressing in the UK, where an overwhelming 71% of pharmacists revealed that incomplete prescriptions are part of their daily reality. For them, what should be a straightforward process of dispensing medication often turns into a daily exercise in catching mistakes, clarifying missing details, and ensuring that patient safety is not compromised. This constant need for correction adds strain to already demanding workflows and creates unnecessary delays for patients.
In Canada, the picture is slightly more varied, but no less concerning. 40% of pharmacists said they receive incomplete prescriptions every single day, while another 40% encounter them occasionally. This inconsistency means that even if a pharmacist escapes the problem on some days, they can always expect it to return, disrupting their routine and demanding extra vigilance.
Moving to Italy, the challenge takes on a different shape. Here, 36% of pharmacists reported dealing with incomplete prescriptions daily, while nearly half (45%) said they encounter them weekly. Though not as constant as in the UK, the fact that the majority experience these issues at least once a week suggests that prescribing gaps are deeply embedded in everyday practice.
However, in Germany, pharmacist confirmed that incomplete prescriptions do occur, albeit occasionally. This reinforces that the problem is not limited to certain healthcare systems but extends across borders, affecting pharmacists in varying ways.
Plan of Action for Pharmacists: These insights are a reminder of just how critical their role is in safeguarding patients. Incomplete medical prescriptions may arrive at their counters every day, but each one presents an opportunity to step in and prevent errors from reaching the patient.
This means pharmacists must remain proactive. They must take out time to verify missing details, reaching out to prescribers for clarification, and documenting recurring issues that could point to larger systemic gaps.
The Prescription Errors Pharmacists See Too Often
Through our survey, pharmacists were also asked about the types/examples of prescription errors they most frequently encounter, and their insights reveal a set of recurring pitfalls that continue to undermine safe prescribing practices.
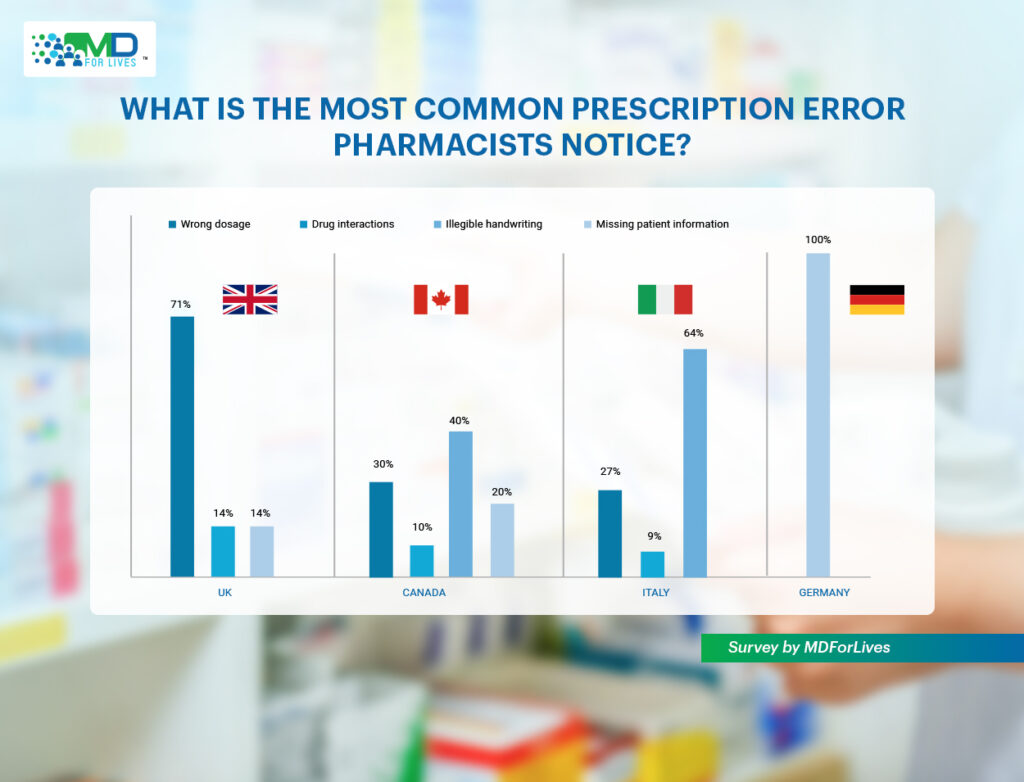
In the UK, the issue of wrong dosage stood out as the most pressing concern, with most pharmacists. An alarming 71% pointed to it as a frequent problem. Italy followed closely, where over a quarter of pharmacists reported dosage errors, while in Canada, 30% of pharmacists said they face the same challenge. Despite advances in prescribing systems, ensuring the right dosage remains a persistent hurdle across regions.
Another age-old problem continues to plague pharmacists – illegible handwriting. In Italy, 64% of pharmacists identified poor handwriting as the most common prescription error they encounter, while in Canada, 40% echoed the same frustration. Even in the era of electronic health records, the simple act of interpreting a handwritten prescription can still jeopardize patient safety.
In Germany, the most pressing issue that emerged was missing patient information. This detail may seem small but can have significant consequences for safe dispensing. However, this concern was not confined to Germany alone; pharmacists in both Canada and the UK also pointed to incomplete patient details as a recurring problem.
Alongside this, some pharmacists highlighted concerns around drug interactions. This acts as a reminder that prescribers are not always fully attentive to how different medications might conflict when combined.
Plan of Action for Pharmacists: To address prescription errors, pharmacists need to adopt a proactive and systematic approach. Verifying unclear dosages and cross-checking for missing details should become standard practice before dispensing, even if it means pausing to consult the prescriber.
Maintaining clear documentation of recurring prescription errors in pharmacy can help identify patterns that warrant wider discussion with medical teams or healthcare institutions.
Is ‘Collaboration’ the Missing Link in Preventing Prescription Errors?
Absolutely! We do feel that one of the simplest yet most powerful solutions to reducing prescription errors in pharmacy lies in stronger collaboration between prescribers and pharmacists.
Pharmacists bring specialized knowledge of drug interactions, side effects, and dosing that can significantly improve patient safety if tapped into consistently. When prescribers actively consult pharmacists, prescriptions are less likely to contain gaps or dangerous oversights, and patients receive safer, more effective care.
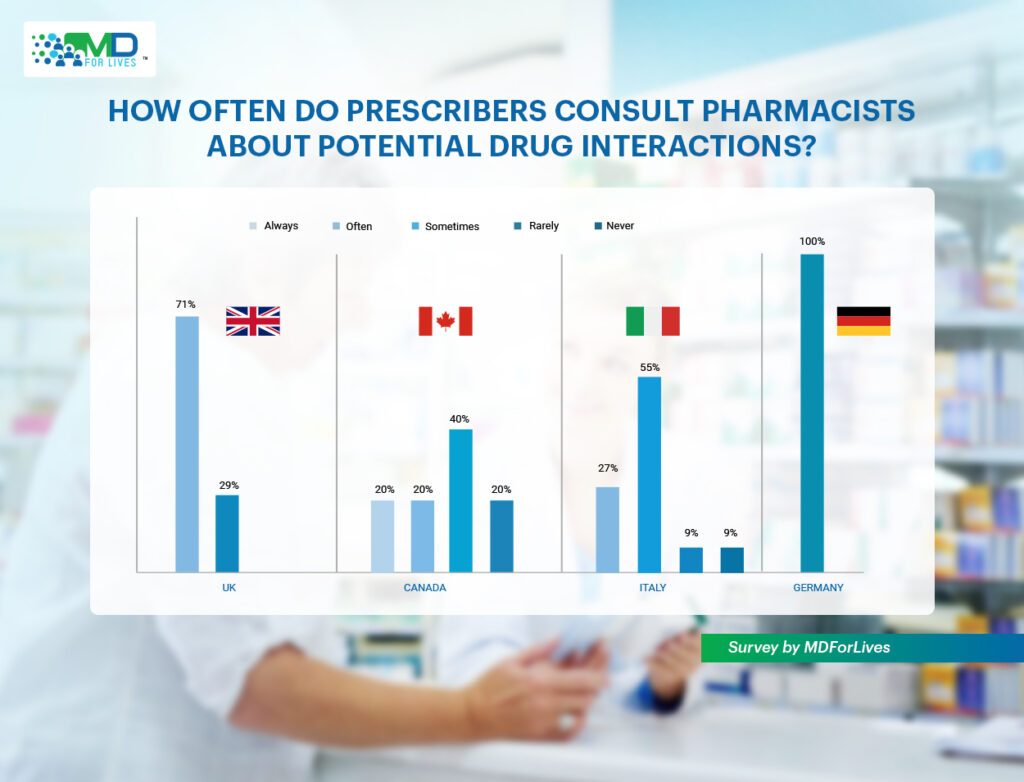
Yet, our survey shows that this collaboration is far from universal. In the UK, 71% of pharmacists said prescribers often consult them about potential drug interactions. Now that is a promising sign of partnership. In Italy, however, more than half reported that such consultations happen only sometimes, suggesting inconsistent engagement.
Canada on the other hand revealed a split picture. 20% of pharmacists said they are always consulted, while 40% said it only happens occasionally.
Meanwhile, in Germany, pharmacists reported that consultation was rare, with prescribers seldom seeking pharmacist input.
Core Insight: These patterns point to a collaboration gap – a missed opportunity to strengthen patient safety by making better use of pharmacists’ expertise. Closing this gap could transform prescription workflows from reactive problem-solving to proactive error prevention, creating a safer healthcare environment for everyone.
Final Thoughts
As we look toward 2025 and beyond, it is evident that healthcare can no longer afford to view prescription errors as the responsibility of one individual or profession alone. The risks posed by incomplete and erroneous prescriptions are too great, and the consequences for patients, too serious to leave unchecked. The path forward must be rooted in shared responsibility, where prescribers and pharmacists work in tandem, not in silos.
Once this gap is bridged, healthcare systems can transform prescribing from a point of vulnerability into a system of reliability and trust. Every prescription, when reviewed with vigilance, can be more accurate and safer.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.