When the heart is unable to pump enough blood and oxygen to keep the body’s other organs alive, heart failure ensues. Although heart failure is a serious illness, it does not always imply that the heart has ceased beating. Congestive heart failure (CHF) is a chronic, progressive illness that reduces your heart muscle’s pumping power. While commonly referred to as “heart failure,” CHF specifically refers to the stage at which fluid accumulates within the heart, causing it to pump inefficiently. The Global Heart Failure Awareness Programme is creating a unified strategy across Europe and beyond to increase heart failure awareness among key audiences.
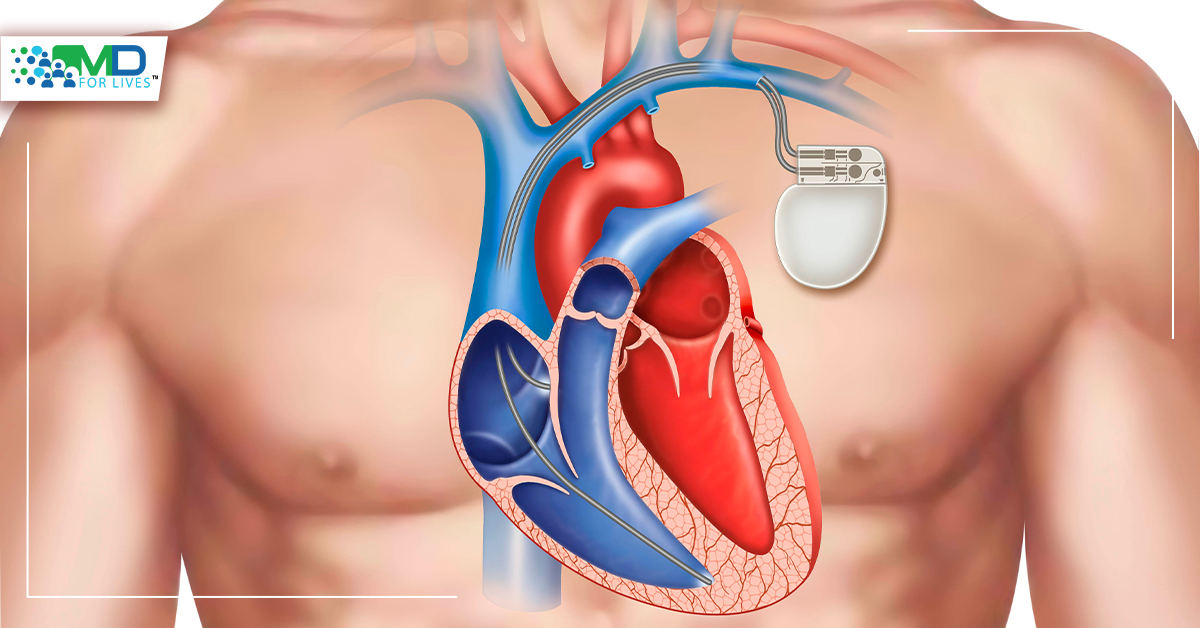
Cardiac Disorders & Pacemakers
Certain cardiac disorders, such as that of restricted arteries in the heart (coronary artery disease) or high blood pressure, cause the heart to weaken or stiffen over time, making it unable to effectively fill and pump blood. Proper therapy can help some individuals live longer by reducing the signs and symptoms of heart failure. Heart Failure Awareness Week is February 14–20 and the public and relevant organisations are encouraged to participate by supporting society’s efforts to raise heart failure awareness, patient education, and prevention. Losing weight, exercising, limiting salt (sodium) in diet, and managing stress are few examples of lifestyle changes that can enhance the quality of life. Heart failure, on the other hand, can be fatal.
Shortness of breath, weariness, swelling legs, and a quick pulse are all symptoms. Eating less salt, decreasing fluid intake, and using prescription medicines are some of the treatments available. A defibrillator or pacemaker may be installed in some situations. Heart failure can cause severe symptoms, in which people may require a heart transplant or a ventricular assist device (VAD).
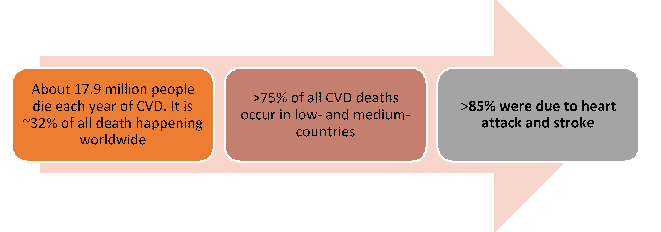
The number of people who died from any cause of sudden cardiac arrest in the US in 2018 was 393,872. According to 2019 research, the majority of OHCAs (Out of Hospital Cardiac Arrests) occur at home: a house or dwelling (70.0%); the most common were public places (18.8%) and nursing homes (11.2%). The majority of cardiovascular diseases may be avoided by addressing behavioural risk factors such as tobacco use, smoking, poor nutrition and obesity, physical inactivity, and alcoholism. It is critical to recognize the cardiovascular disease as soon as possible so that treatment may begin with counselling and medications.
This year, a revolutionary pacemaker that restores the heart’s naturally erratic pulse will be trialled in New Zealand cardiac patients. When we look at the frequencies in our heart rate, we can see that it is linked to our breathing. It rises with inspiration and falls with expiration, and this is a common occurrence in both animals and humans. The function of this variability was determined to be investigated by scientists. They developed a mathematical model that anticipated energy savings. This led them to wonder why a metronomic pulse was employed in energy-depleted heart failure patients.
Heart Rate Variability and Bionic Pacemaker
Heart rate variability is lost in all cardiovascular disease patients, which is an early warning that something is amiss. The heart rate of those with high blood pressure or heart failure is not controlled by their breathing. It may be a little, but it’s depressed and repressed to a great extent. Researchers decided to reintroduce heart rate variability into animals suffering from heart failure to determine whether it helped. The most recent published research was on a large animal model of heart failure, following positive signals in rats. The good news is that scientists have discovered a mechanism to reverse heart failure.
There is currently no treatment for heart failure available on the market. The only thing the medicines will do is to make you feel better. They do not address the fact that you have injured tissue that is not contracting as well as it once did. The new pacemaker restores this variability, which is normal and can be referred to as “nature’s pacemaker.” Pacemakers now produce a metronomically stable heartbeat, but research suggests that injecting natural variation in the heartbeat increases the heart’s capacity to pump blood throughout the body. The second important news is that they have a 20% increase in cardiac output, which is the heart’s ability to pump blood throughout the body. And 20% is a significant figure. The pacemaker resembles a bionic device in appearance. It recognizes the signals from the body that indicate when the gadget is breathing in and out. The gadget must then communicate with the body, pacing the heart up during inhalation and down during exhalation.
A cardiologist at Auckland’s Middlemore Hospital described the findings as “very interesting.” Permanent pacing is ‘non-physiological’ to some extent, and pacing-induced cardiomyopathy is a well-known condition, recognized clinically. It will be fascinating to see if the results are applicable to people. Dr. Martin Stiles, the trial’s principal cardiologist from Waikato Hospital in Hamilton, New Zealand, said: “Current pacemakers normally enhance cardiac function, but this bionic pacemaker has well above our expectations. This breakthrough might change the way heart failure patients are treated in the future.” The next stages are already underway, with plans to enroll patients for a clinical study in New Zealand later this year.
Read also