Shingles, or herpes zoster, occurs when the dormant varicella-zoster virus (the same virus that causes chickenpox) is reactivated in the body. This often occurs in times of stress or when the immune system is weakened.
Shingles rates have been increasing in the US for several decades. Doctors have recently noted an increase in shingles cases among younger adults, but the reason for this rise in cases is still under investigation. Other recent research suggests that people over 50 who recently had COVID-19 may have a higher risk of developing shingles.
What is Shingles?
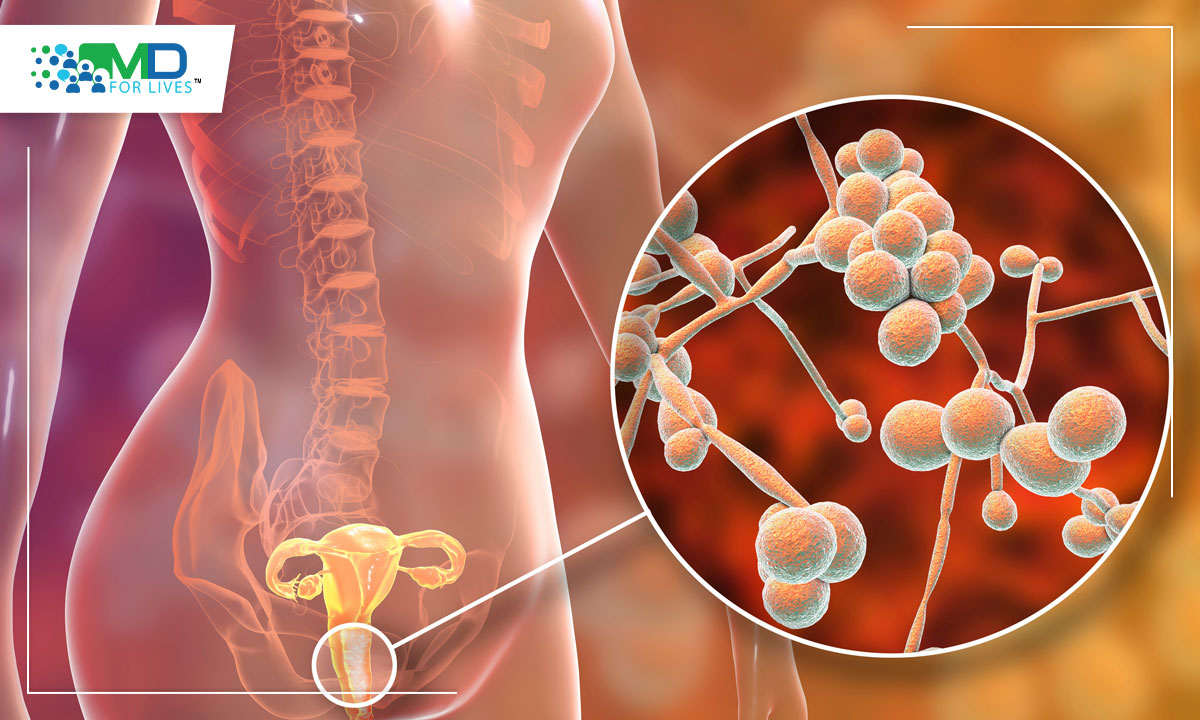
After recovery from chickenpox, the varicella-zoster virus remains dormant in the nerves. Later in life, the latent virus can be reactivated, causing shingles (also known as herpes zoster). In shingles, the reactivated virus infects the nerves that lead to the skin, causing painful skin inflammation and blistering, most frequently in the chest, back, or abdomen. In some cases, shingles leads to postherpetic neuralgia (persistent pain at the site of the rash), and loss of vision can occur if the rash affects the eye.
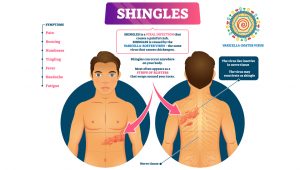
Image caption: Shingles is caused by the reactivation of the varicella-zoster virus causing painful skin inflammation and blistering mostly in the chest, back, or abdomen.
What causes the reactivation of the varicella-zoster virus?
A weakened immune system that cannot maintain the latency of the virus seems to be the main trigger for the reactivation of the varicella-zoster virus. This might explain the increased incidence of shingles among people older than fifty and among individuals who are immunocompromised or using immunosuppressants.

Shingles cases rising among young adults
Over a lifetime, one out of 3 adults in the US develops shingles, and it is estimated that 1 million people develop shingles every year. In the last 60 years, the incidence of shingles rates has been increasing steadily in the US, even among young adults. The incidence of shingles between 1945 and 1949 was 0.76 per 1000 people, whereas from 2000 to 2007, the incidence was 3.15 per 1000 people. Among the elderly, the incidence increased by 39% from 1992 to 2010.
Why is shingles incidence increasing?
It is not completely clear why there has been an increase in the incidence of shingles. Strangely, one possible reason is the development of the chickenpox vaccine, which lowered the US incidence of chickenpox by 90% after it was introduced in 1995.
According to the exogenous boosting theory, being re-exposed to the varicella virus by being in contact with children who have chickenpox prevents the reactivation of the virus. If chickenpox vaccination reduces the number of adults exposed to children carrying the virus, with time, the immune system could lose its vigilance toward this virus. Hence, people who had chickenpox in childhood could become susceptible to developing shingles at an earlier age. A 2013 review details evidence from multiple studies that exogenous boosting can likely explain some, but not all, of the recent increases in shingles incidence.
Another possible reason for the increase is the increased number of people living with compromised immune systems. However, this cannot account for the increase in the number of young healthy people who get shingles.
The connection between Shingles and COVID-19 infection
Several published medical reports have highlighted a potential connection between COVID-19 infection and shingles.
In Brazil, public health data showed a 35.4% increase in the number of cases of shingles between March and August 2020 compared with the same periods from 2017 to 2019. In Turkey, cases of shingles between May and June 2020 doubled compared with the same period in 2019.
The authors of a retrospective cohort study published in March 2022 in Open Forum Infectious Diseases investigated a possible connection between diagnosis of COVID-19 and shingles among people older than 50. They analyzed data from nearly 400,000 patients who had received a COVID-19 diagnosis and over 1.5 million people who had not. They found that compared to matched controls, people diagnosed with COVID-19 had a significantly higher risk of developing shingles (15% higher) after their COVID-19 infection, and those who were hospitalized for COVID-19 had a 21% higher risk than control patients.
The importance of Shingles Vaccination
Vaccination rates for shingles dropped during the COVID-19 pandemic. Even after the pandemic wanes, the need will remain. Increasing vaccination rates will pay off. The herpes-zoster vaccine used in the US can reduce the risk of developing shingles by over 90% for those with healthy immune systems and by 68-91% for those with various immune system disorders.


MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.