Chronic kidney disease (CKD), a global public issue is associated with substantial morbidity and mortality. In the past few decades, the prevalence of chronic kidney disease has increased significantly with the high cost and poor outcomes.
In 2017, the global prevalence of CKD was found to be 9.1% (697.5 million cases), resulting in 1.2 million deaths. Also, CKD, the important risk factor of cardiovascular disease (CVD) accounted for 7.6% (1.4 million) of all CVD deaths in 2017.[1]
The Global Prevalence of Disease (GBD) studies (2016,2017) suggest the prevalence of CKD is higher in women than men.[1][2] However, the male gender is associated with more rapid progression of CKD.[3]
CKD is generally progressive and irreversible, but potentially preventable. Identifying the precursors such as diabetes, hypertension, etc. can prevent the development of CKD or delay the progression and complications of CKD.
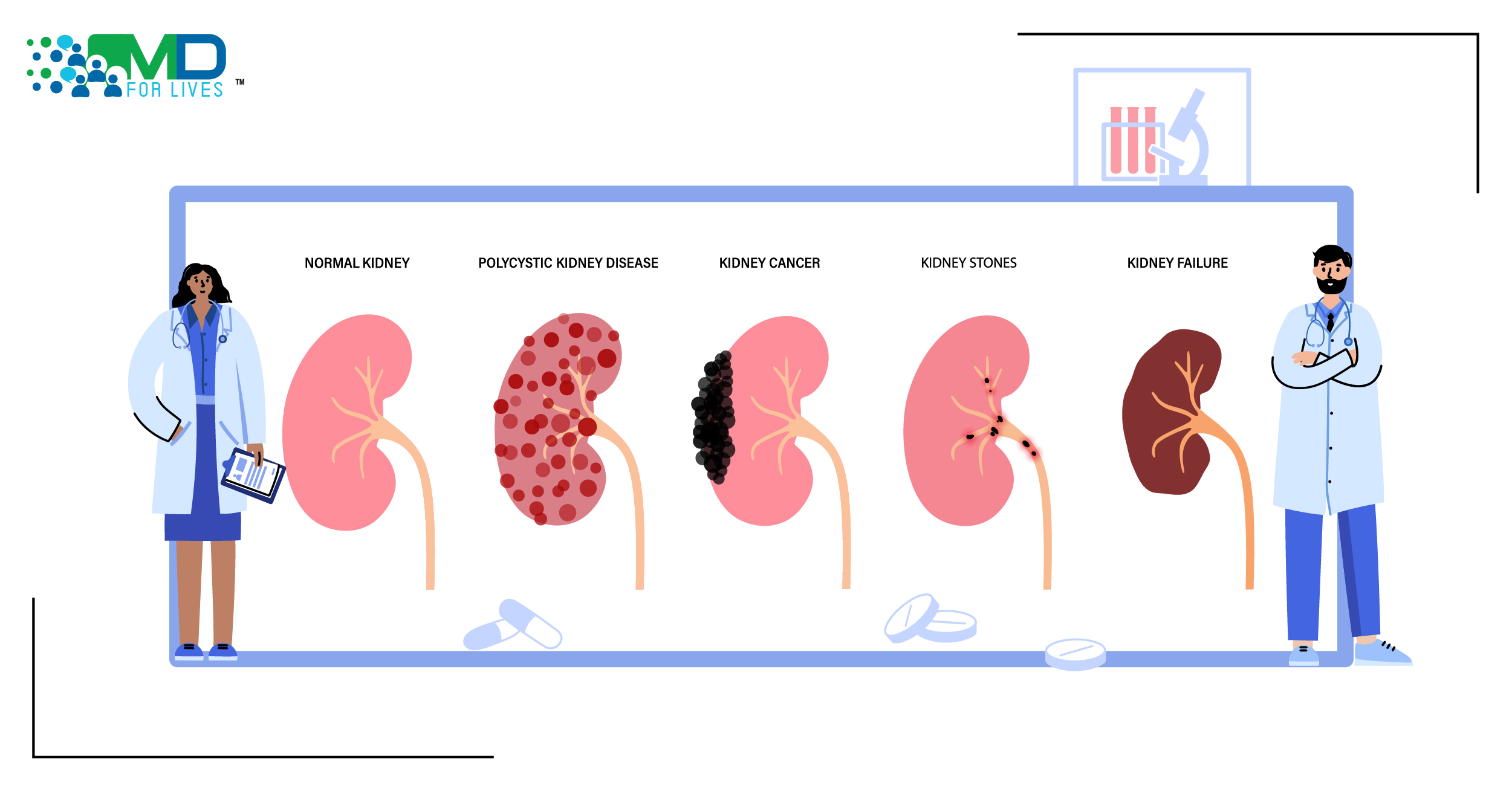
Understanding Chronic Kidney Disease
Guidelines define chronic kidney disease as kidney damage or estimated glomerular filtration rate (eGFR) less than 60 ml/min/1.73 m2, for at least 3 months.
CKD is usually asymptomatic till stages IV and V. Increased urinary albumin excretion- the albuminuria is a marker of kidney damage. The classification and staging of CKD is based on the GFR and albuminuria.[4]
CKD is a major concern for the aging population, as it is associated with age-related functional decline accelerated in metabolic syndrome.[5]
Renal impairment can significantly increase the risk of cardiovascular diseases and CKD is considered an independent risk factor for cardiovascular diseases. Individuals with CKD are more likely to die from coronary artery disease than progress to end-stage renal disease (ESRD).[6]
Early detection, evaluation, and management can prevent/slow the progression- can prevent kidney damage and cardiovascular diseases.
The healthcare cost of CKD care is high particularly for dialysis, transplantation, and cardiovascular disease management.

Risk Factors of Chronic Kidney Disease
Major non-modifiable risk factors include genetic make-up, older age, non-Caucasian ethnicity, low-birth weight, and family history of CKD or CVD.[7] Metabolic syndromes such as hypertension, diabetes mellitus, obesity, and dyslipidemia, and also the smoking has been identified as the leading modifiable risk factors for the development and progression of CKD.[8]
Hypertension is the leading cause of ESRD and has been associated with the complications of CKD.[4]
Screening is recommended for the high-risk population including patients with diabetes, hypertension, and people above 65.[4]
Evaluation of Chronic Kidney Disease
The evaluation includes the assessment of GFR (measuring serum creatinine level) and proteinuria (urinary albumin/creatinine ratio), and imaging of kidney such as ultrasound, renal ultrasound Doppler, computerized tomography, renal angiography, voiding cystourethrography, etc.[4]
Urinalysis helps to detect glomerulonephritis, vasculitis, tubulointerstitial disease, lupus nephritis, etc.[9]
Treatment Strategies to Slow Progression and Reduce Complications of CKD
Risk of progression of CKD include diabetes, hypertension, increasing albuminuria, decreasing eGFR, etc.[10]
Frequent monitoring of urine albumin-to-creatinine ratio and eGFR to evaluate the progression of the disease and treatment response helps to manage CKD.[10]
(a)Medical Management
Diabetes management – Persistent blood glucose control may reduce the development of kidney disease.[8]
Blood pressure control –Antihypertensive therapy for hypertension can reduce the morbidity and mortality in CKD. Regular monitoring and treating hypertension is an effective intervention.
Angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are the first-line drugs for hypertension and proteinuria/albuminuria.[8][10]
(b)Dietary and Lifestyle Modifications
Dietary and lifestyle modifications can reduce the risk associated with metabolic syndrome.
Weight loss, a low-sodium diet, low-fat dairy products, dietary protein restriction can reduce high blood pressure and albuminuria.
Smoking, the component of metabolic syndrome and the risk factor of CKD, CVD, etc., is associated with albuminuria/proteinuria and decreased GFR.[8][11]. Reduced physical activity in dialysis and CKD patients can increase the risk of morbidity and mortality.[12]
Renal Replacement therapy such as dialysis and kidney transplantation is recommended for progressive/advanced kidney disease.

- https://www.nature.com/articles/s41581-020-0268-7
- https://www.karger.com/Article/FullText/489897
- https://jasn.asnjournals.org/content/jnephrol/30/1/137.full.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK535404/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4934905/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055978/
- https://www.sciencedirect.com/science/article/pii/S2157171615311734
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3088518/
- https://www.aafp.org/afp/2011/1115/afp20111115p1138.pdf
- https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/identify-manage-patients/manage-ckd/monitor-progression
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342637/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7066543/