The interplay between the thyroid gland and the brain represents a nexus of extraordinary significance in human physiology. Often revered for its role in metabolic regulation, the thyroid’s influence extends beyond energy balance, reaching into the delicate mechanisms governing cognitive function. This bidirectional relationship, the thyroid-brain axis, captivates our attention during this thyroid awareness month.

Thyroid-brain axis is a pivotal juncture in medical science, where the subtle intercommunications between the thyroid gland and the brain cast profound shadows on cognitive health. Within this discourse lies a profound understanding that transcends conventional perspectives, shedding light on how thyroid hormones wield their influence far beyond the boundaries of metabolism, intricately shaping our thoughts, moods and cognitive processes.
Explore further for a comprehensive insight into thyroid cognitive problems and discover strategies empowering physicians to elevate patient care.
Thyroid-Brain Axis: Understanding The Bidirectional Relationship
At its core, this bidirectional relationship involves the thyroid gland, responsible for producing hormones essential for regulating metabolism and the brain, orchestrating neurological functions. Thyroid hormones, predominantly thyroxine (T4) and triiodothyronine (T3) play a pivotal role in metabolic processes and in shaping brain development, neuronal differentiation and synaptic function.
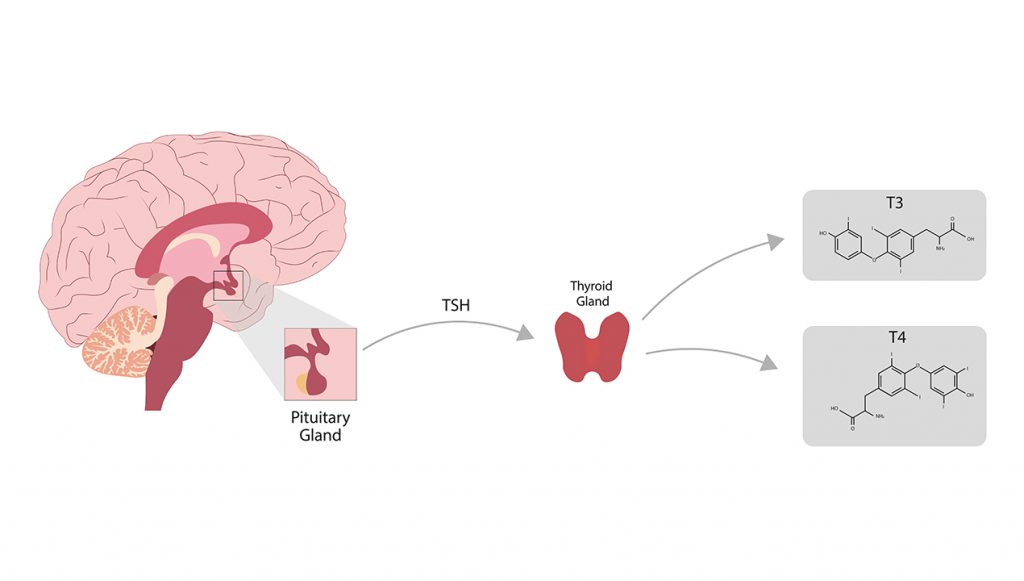
Conversely, the brain exerts control over the thyroid gland through the hypothalamus-pituitary-thyroid (HPT) axis. This regulatory pathway involves the hypothalamus releasing thyrotropin-releasing hormone (TRH), which stimulates the pituitary gland to secrete thyroid-stimulating hormone (TSH). Subsequently, TSH prompts the thyroid to produce T4 and T3, completing the feedback loop that governs hormone levels and their impact on the brain.
Comprehending the interconnectedness between thyroid and brain function unveils insights into cognitive impacts is essential to aiding comprehensive patient care by integrating thyroid function with neurological assessments for a holistic approach to evaluating thyroid cognitive problems.
Thyroid Gland: An Overview of its Impact on Cognitive Function
The thyroid’s impact on cognitive function is significant. Imbalances in thyroid hormones, whether too little (hypothyroidism) or too much (hyperthyroidism), can lead to cognitive issues.
- Hypothyroidism

Hypothyroidism leads to difficulties in memory, learning, focus, decision-making, attention, language and executive functions. The brain lacks the necessary energy for functions and causes changes in the hippocampus, a brain region crucial for cognition.
Please note: While global data on the prevalence of cognitive impairment among hypothyroid patients is lacking, multiple studies from diverse regions suggest its common occurrence. Reports indicate that cognitive impairment affects approximately 17% in Minnesota, 28% in Los Angeles and 32% in India among individuals with hypothyroidism.
- Hyperthyroidism

Excessive thyroid hormone production in hyperthyroidism correlates with cognitive decline, particularly dementia in the elderly. Research indicates a 12% increased risk of dementia over six months with hyperthyroidism. Graves’ disease, a common cause of hyperthyroidism in older individuals, is notably linked to a higher incidence of dementia.
Both hypo- and hyperthyroidism significantly impact cognition, highlighting the crucial importance of comprehending and managing thyroid disorders to prevent cognitive complications.
Key Strategies for Physicians to Enhance Thyroid-Brain Axis Management

Here are a few essential strategies empowering physicians to navigate and address thyroid cognitive problems effectively:
- Personalized Treatment Plans
Tailor thyroid hormone replacement therapies based on individual patient response and needs. For example, adjusting dosage according to age, comorbidities and specific cognitive symptoms can optimize outcomes. Customizing treatment plans may involve prescribing levothyroxine or considering combination therapies like T3 and T4 for certain patients.
- Cognitive Assessments and Follow-Ups
Incorporate routine cognitive assessments alongside thyroid function tests during follow-up visits. Implement standardized cognitive screening tools like the Montreal Cognitive Assessment (MoCA), a highly sensitive tool for early detection of mild cognitive impairment, or Mini-Mental State Examination (MMSE), a valuable and systematic tool for a comprehensive assessment of mental status, particularly beneficial when evaluating older adults.
- Lifestyle Modifications
Advocate lifestyle adjustments that complement medical interventions. Encourage a balanced diet rich in iodine, selenium and other essential nutrients crucial for thyroid and cognitive function. Promote regular exercise and stress management techniques, as stress can impact thyroid and brain function.
- Collaborative Care Networks
Establish partnerships with mental health professionals to address cognitive symptoms. For instance, working with neuropsychologists or psychiatrists can aid in identifying and managing mood disorders or cognitive deficits associated with thyroid dysfunction.
- Utilizing Telemedicine and Remote Monitoring
Integrate telemedicine platforms for remote consultations and monitoring. Employ telehealth tools for regular check-ins and to remotely assess symptoms. For example, leveraging smartphone applications that track mood fluctuations or cognitive exercises for at-home assessment.
- Patient Education Programs
Conduct educational workshops or provide informational materials to patients and their families. Explain the relationship between thyroid and brain function, emphasizing the importance of treatment adherence and recognizing early signs of cognitive changes.
- Clinical Research Participation
Encourage patient involvement in clinical trials focused on thyroid and cognitive function. Engaging patients in research offers them access to potential cutting-edge treatments and contributes to advancing medical knowledge in this field.
- Continuous Professional Development
Participate in conferences, workshops and online courses specializing in the thyroid-brain axis. Accessing peer-reviewed journals and attending seminars keeps physicians updated on emerging trends and breakthroughs in managing thyroid-related cognitive issues.
Conclusion

The bidirectional relationship highlights the importance of considering thyroid function and brain health when addressing cognitive impairments. As research unravels the complexities of the thyroid-brain axis, it offers hope for enhanced diagnostic strategies and tailored treatments, ultimately improving the quality of life for individuals affected by thyroid cognitive problems.
Physicians reading this blog are welcome to engage with MDForLives’ community, committed to catalyzing significant advancements in healthcare. Participating in paid medical surveys and sharing thought-provoking articles or impactful case studies can enrich our community’s knowledge! Join us.
You can also explore opportunities to participate in enlightening webinars and engaging discussion forums, fostering connections within the healthcare sphere while exchanging invaluable insights.
References:
The effect of hyperthyroidism on cognitive function, neuroinflammation and necroptosis in APP/PS1 mice
www.translational-medicine.biomedcentral.com
Cognitive Impairment and Associated Factors Among Adult Hypothyroid Patients in Referral Hospitals, Amhara Region, Ethiopia: Multicenter Cross-Sectional Study
www.dovepress.com
Association of thyroid disease with risks of dementia and cognitive impairment: A meta-analysis and systematic review
www.frontiersin.org

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.