For decades, diabetes has been described as a lifelong condition that can be managed but not cured. Every day, millions of people across the world measure blood sugar, adjust insulin, follow diets, and schedule their lives around glucose fluctuations. This constant vigilance saves lives. However, it also comes with emotional strain, financial burden, and the ever-present fear of long-term complications. But there is good news – science is rewriting that story. Over the past five years, diabetes research has entered one of its most exciting chapters. Advances, once thought to be distant possibilities like stem-cell therapies, gene editing, and “smart” insulin, are now being tested in patients. New immunotherapies are showing that diabetes might be delayed or even prevented! Novel procedures offer alternatives to daily injections and pills. And last but not least, artificial intelligence is helping people fine-tune their diabetes cure treatment in ways never before possible.
What makes this moment different is the speed and scale of progress. Breakthroughs are no longer confined to the laboratory; they are moving into clinical trials, real-world testing, and in some cases, regulatory approval. The question is shifting from ‘if’ a diabetes cure in future is possible to ‘when’ it will become accessible.
The Quest for a Diabetes Cure
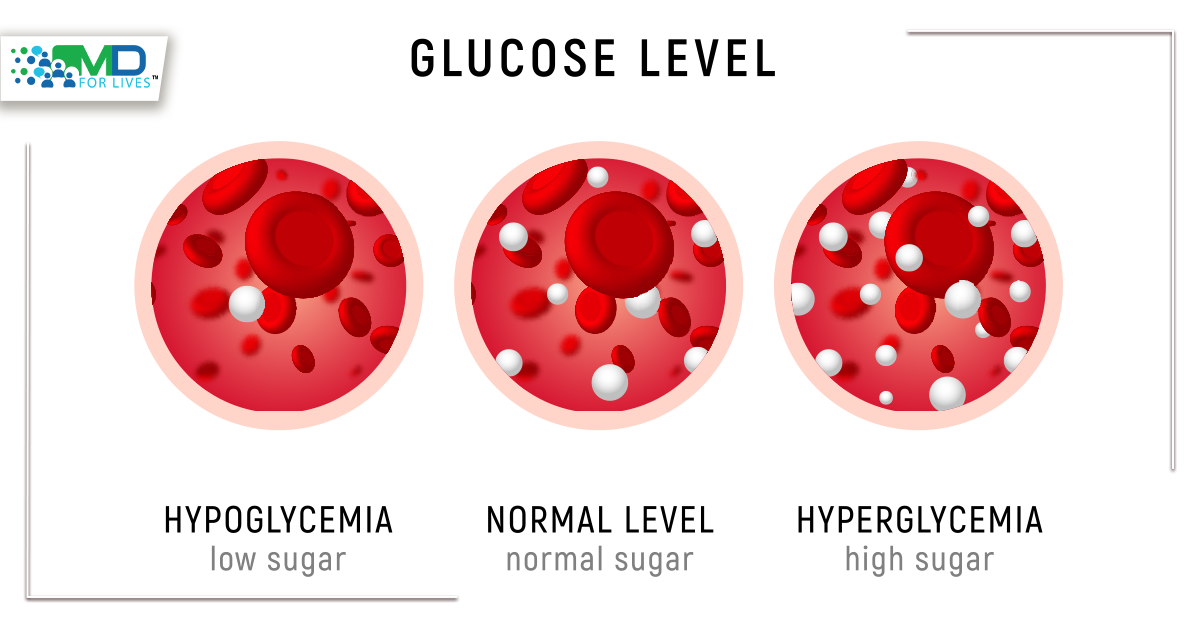
Diabetes is not a single disease but a group of conditions that all revolve around one problem – the body’s inability to regulate blood sugar effectively.
- Type 1 Diabetes is an autoimmune condition where the immune system destroys insulin-producing beta cells in the pancreas.
- Type 2 Diabetes develops when the body becomes resistant to insulin or when the pancreas cannot produce enough of it.
For decades, the focus has been on better management tools, such as insulin injections, glucose monitors, lifestyle modifications, and medications. These tools save lives, but they do not tackle the underlying cause. That is why researchers are chasing diabetes cure therapies that could restore insulin independence, reset the immune system, or even prevent diabetes altogether.
Stem Cells: Rebuilding the Pancreas

One of the most exciting areas of research lies in stem cell therapy. Stem cells are master cells that can develop into any type of cell, including the beta cells that produce insulin.
- Vertex Pharmaceuticals recently reported groundbreaking results in a clinical trial where Type 1 diabetes patients received stem-cell-derived islet cell transplants. One participant achieved near-normal blood sugar control without the need for insulin injections for over a year.
- ViaCyte, another biotech company, is testing an implantable “pouch” containing stem cells that mature into insulin-producing cells once inside the body.
The biggest hurdle? Preventing the immune system from attacking these new cells. Researchers are exploring encapsulation technologies (tiny protective barriers) that let nutrients in but keep immune cells out. If successful, this could be a functional type 1 diabetes cure.
Gene Editing and Immunotherapy: Fixing the Root Cause
For Type 1 diabetes, the real villain is the immune system itself. That is why scientists are using tools like CRISPR gene editing and immunotherapy to reprogram the body.
- Recent clinical trials have shown that a drug called teplizumab can delay the onset of Type 1 diabetes in high-risk individuals by up to two years. It works by calming the immune attack on beta cells.
- In the future, gene editing could go a step further by correcting the immune system’s “mistake” at the DNA level. Though still experimental, this approach has the potential to prevent Type 1 diabetes entirely.
These therapies are less about replacing what’s lost and more about stopping the disease before it progresses.
Smart Insulin and the Artificial Pancreas
Even without a full diabetes cure, new technologies are making life dramatically easier for people with diabetes.
- Smart Insulin: Researchers are developing insulin that activates only when blood sugar rises, reducing the risk of dangerous highs and lows. Imagine injecting once and letting the insulin “think” for you.
- Artificial Pancreas Systems: Powered by continuous glucose monitors and insulin pumps, these closed-loop devices automatically adjust insulin delivery in real time. Many patients report that it feels like getting their life back.
In fact, the FDA has already approved hybrid closed-loop systems, and next-generation fully automated versions are under review. These are not technically cures, but they get very close to restoring natural blood sugar control.
The Gut Connection: Rethinking Type 2 Diabetes
While Type 1 diabetes cure research focuses on immunity, curing Type 2 diabetes has sparked another fascinating direction – the role of the gut.

- Bariatric (weight-loss) surgery has shown that in many patients, blood sugar levels return to normal within days, long before significant weight loss occurs. This suggests that altering gut hormones can reset metabolism.
- Drugs like GLP-1 receptor agonists (Ozempic, Mounjaro, etc.) mimic these gut hormones and are now revolutionizing Type 2 diabetes care. They improve blood sugar, aid weight loss, and even reduce the risk of heart disease.
- Researchers are also studying how the gut microbiome (trillions of bacteria) in our intestine might hold the key to preventing or reversing diabetes.
This gut-based research is shifting the focus from managing symptoms to reprogramming metabolism at its core.
How Close Are We to a Diabetes Cure?
The big question on everyone’s mind is simple – “How close are we to ending diabetes once and for all?” The honest answer is that we are closer than ever before! Yet, the finish line is still ahead.
For Type 1 diabetes cure, the progress is striking. Stem-cell-derived islet cell transplants have allowed some patients to live without insulin for months, even years, marking the first time true insulin independence has been restored outside of an organ transplant. Immunotherapies like teplizumab are showing that it’s possible to delay or even prevent the onset of Type 1 diabetes in high-risk individuals. These diabetes cure therapies are no longer just “ideas on paper,” they are in late-stage clinical trials, and some are already being reviewed by regulators.
That said, the hurdles are real: Keeping the immune system from attacking new cells, ensuring long-term durability of the treatments, and making them scalable for millions of patients.
For curing Type 2 diabetes, the lines between treatment and reversal are starting to blur. Bariatric surgery has long shown that in many cases, blood sugar normalizes within days of the procedure, well before significant weight loss occurs, hinting at powerful metabolic shifts in the gut. Now, medications that mimic these effects, such as GLP-1 receptor agonists and dual incretin drugs, are helping people achieve remission without surgery. Some patients are able to stop diabetes medications altogether, maintaining normal glucose levels through these therapies. While not technically a “diabetes cure,” the possibility of remission is offering new hope to millions living with Type 2 diabetes.
Technology is also playing a transformative role. Artificial pancreas systems that use continuous glucose monitoring and automated insulin delivery are already available and giving patients what many describe as a “functional diabetes cure.” While users still depend on devices, the burden of constant decision-making is dramatically reduced, offering something remarkably close to natural blood sugar regulation.
Despite this progress, the path forward is not without obstacles. Scientific breakthroughs must pass the tests of long-term safety, real-world effectiveness, and affordability. A therapy that works in a small group of trial participants must be proven across diverse populations, cultures, and healthcare systems. And even when effective, treatments must be made financially accessible. Otherwise, they risk being life-changing for a few, but out of reach for many.
The Road Ahead
What is remarkable about this moment in diabetes research is the sense of momentum. Scientists, biotech companies, and patient advocates are collaborating like never before. Major funding is flowing into clinical trials, and early results are promising.
Still, patience is necessary. Translating laboratory breakthroughs into everyday treatments takes time (often years or even decades). But the fact that some patients are already insulin-free through experimental therapies shows that the idea of a diabetes cure is becoming real.
FAQs
Q1. Is there a permanent cure for diabetes?
Currently, there is no permanent diabetes cure, but science is closer than ever. Stem cell therapies, gene editing, and gut microbiome research are showing promising results in both type 1 diabetes cure and curing type 2 diabetes through remission.
Q2. How close are we to a type 1 diabetes cure?
Clinical trials in stem-cell-derived islet cell transplants have allowed some patients to live without insulin for over a year. Immunotherapies like teplizumab are delaying or even preventing the onset of Type 1 diabetes. While not yet a universal cure, these advances are a major step forward.
Q3. Can type 2 diabetes be cured naturally?
There is no guaranteed natural cure for type 2 diabetes, but many people achieve remission through lifestyle changes, bariatric surgery, or therapies that target the gut microbiota and diabetes connection. Medications like GLP-1 receptor agonists are also helping patients stop insulin and maintain healthy glucose levels.
Q4. Will I always need insulin for diabetes?
Not always. In type 1 diabetes, insulin is usually essential, but stem cell and gene therapies may change this in the future. In type 2 diabetes, some patients can reduce or even stop insulin through weight loss, surgery, or advanced medications.
Q5. What role does the gut play in curing diabetes?
Research shows that the diabetes gut microbiome may influence metabolism, insulin sensitivity, and even the progression of Type 2 diabetes. Bariatric surgery and gut hormone–based drugs are helping some patients achieve remission, highlighting the importance of gut microbiota in diabetes treatment.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.