Every year on July 28th, the world comes together to observe World Hepatitis Day, raising awareness about viral hepatitis and the urgent need for global action. This significant day serves as a call to action for hepatologists worldwide to unite in the fight against this silent killer that affects millions of people.
Burden of Viral Hepatitis
Viral hepatitis is a group of infectious diseases caused by hepatitis viruses (A, B, C, D and E), each posing unique challenges to public health. Among these, hepatitis B and C are the most dangerous, as they can lead to chronic infection, cirrhosis, liver failure and even liver cancer if left untreated. According to the World Health Organization (WHO), approximately 325 million people worldwide are living with chronic hepatitis infections, and many are unaware of their condition.
Despite being preventable and treatable, viral hepatitis continues to claim around 1.4 million lives each year, making it a major global health concern. It is estimated that only a small fraction of those in need have access to testing, treatment and care. Hepatologists play a pivotal role in addressing these challenges by providing expertise, conducting research and advocating for improved healthcare policies and resources.
Acute Liver Failure Secondary to Autoimmune Hepatitis
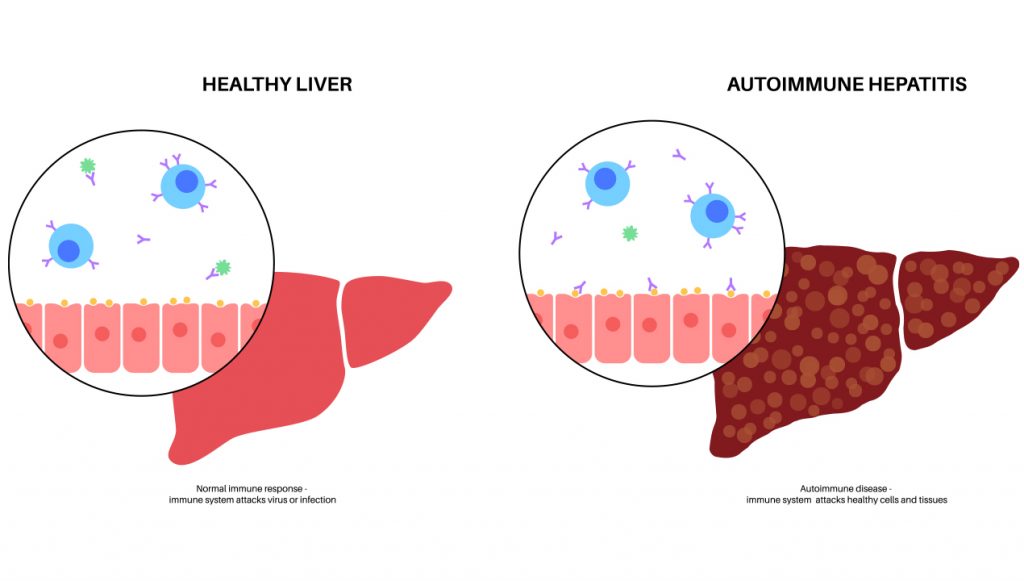
Autoimmune hepatitis is an inflammatory liver disease of unknown cause that can lead to severe complications, including liver cirrhosis and end-stage liver failure if not promptly diagnosed and treated. The clinical presentation varies, with some cases resembling acute hepatitis, while others may remain insidious or asymptomatic. It affects individuals of all ages but is more common in women, with its incidence seemingly on the rise worldwide. The disease’s pathogenesis involves an abnormal immune response targeting liver autoantigens, resulting in persistent and self-perpetuating liver inflammation.
Diagnosing autoimmune hepatitis requires the identification of specific autoantibodies, elevated IgG concentrations and characteristic histological features of interface hepatitis and periportal necrosis. Swift response to treatment with corticosteroids and immunomodulatory drugs is typically observed, supporting the diagnosis and aiming to induce and maintain long-term remission of liver inflammation. Moreover, treatment has shown the potential to reverse liver fibrosis, thereby preventing the progression to advanced cirrhosis and its associated complications.
Despite successful treatment outcomes in most patients, autoimmune hepatitis remains a common cause of acute liver failure. For those who do not respond to initial therapy or develop acute liver failure, treatment involves steroids and may necessitate liver transplantation. A recent study aimed to characterize acute liver failure secondary to autoimmune hepatitis and identify variables predictive of 21-day transplant-free survival.
The study included 193 cases of acute liver failure secondary to autoimmune hepatitis, with 83.4% diagnosed on enrollment and 16.6% developing it during hospitalization. At 21 days, 59.6% underwent liver transplantation, 14.5% experienced transplant-free survival and 23.8% unfortunately succumbed before transplantation. Higher admission values of bilirubin, INR and coma grade were associated with worse outcomes. The study successfully developed a prognostic index incorporating bilirubin, INR, coma grade and platelet count with a concordance statistic of 0.84. This index can aid in predicting 21-day transplant-free survival and identifying patients requiring expedited liver transplant evaluation.
Implications for Diagnosis and Treatment
The implications for the diagnosis and treatment of autoimmune hepatitis are of paramount importance in managing this inflammatory liver disease effectively. Early and accurate diagnosis, based on specific autoantibodies, elevated IgG levels and characteristic histological features, is crucial to initiate prompt treatment and prevent disease progression to severe complications like liver cirrhosis and end-stage liver failure. The timely response to corticosteroid and immunomodulatory therapies further underscores the significance of early intervention. For patients unresponsive to initial treatments or those experiencing acute liver failure, additional therapeutic measures, including steroids and liver transplantation, are essential. The recent study’s prognostic index offers a valuable tool for identifying high-risk patients in need of urgent liver transplant evaluation, potentially improving short-term survival rates. Heightened awareness of autoimmune hepatitis and its diagnostic hallmarks, along with improved treatment strategies, is essential to ensure better patient outcomes and enhance public health.
Call for Collaborative Research
The recent studies on autoimmune hepatitis open up exciting avenues for further research and collaborative studies. Hepatologists, immunologists, autoimmune disease specialists and researchers from the healthcare industry can join forces to delve into the new discoveries and their potential implications.
By pooling expertise and resources, researchers can better understand the underlying mechanisms, identify biomarkers to predict this overlap and develop targeted therapies that address both the viral and autoimmune aspects of the condition. Such collaborative efforts could revolutionize the approach to managing hepatitis patients with autoimmune features, ultimately leading to improved outcomes and a deeper understanding of both conditions.
In this digital age, hepatologists can leverage various platforms to contribute to research. Medical survey platforms have emerged as an excellent way for doctors, including hepatologists, to participate in important studies, share their insights and contribute to medical advancements. These platforms connect medical professionals with researchers conducting studies related to hepatitis and other liver diseases.
By signing up with reputable medical survey platforms, hepatologists gain access to a wide range of surveys and research projects related to viral hepatitis. Participating in these surveys not only allows hepatologists to stay up-to-date with the latest research but also empowers them to actively contribute to the scientific community.

Unlocking Lucrative Opportunities for Hepatologists with MDforLives
MDforLives, a premier platform for medical professionals, offers hepatologists and other physicians exciting opportunities to diversify their careers and boost their income. Through the platform, physicians can engage in highest-paid surveys, sharing their expertise and contributing to cutting-edge research while earning generous compensation. Moreover, they can become paid writers for blogs and case studies, showcasing their knowledge to a global audience, and even secure paid speaking engagements at webinars. As an added benefit, hepatologists gain free access to the latest blogs, newsletters and case studies authored by expert physicians and other medical professionals, empowering them to stay at the forefront of medical knowledge and advancements.
Conclusion:
The world of hepatology is continuously evolving, and recent discoveries have unearthed many hidden facts. These emerging discoveries challenge conventional wisdom, offering new insights into the complexities of these conditions. As we embark on this uncharted territory, collaboration among medical disciplines becomes paramount. By fostering a united effort between hepatologists, immunologists, autoimmune specialists and researchers, we can illuminate the underlying mechanisms, improve diagnostic accuracy, tailor treatments and ultimately pave the way for more effective and personalized care for patients living with hepatitis and autoimmunity.
References:
- New hepatitis data highlight need for urgent global response. www.who.int. Accessed July 27, 2023.
- Jefferies M, Rauff B, Rashid H, Lam T, Rafiq S. Update on global epidemiology of viral hepatitis and preventive strategies. World Journal of Clinical Cases. 2018;6(13):589-599.
- Muratori L, Ansgar Wilhelm Lohse, Lenzi M. Diagnosis and management of autoimmune hepatitis. Published online February 6, 2023:e070201-e070201.
- Enke T, Livingston S, Rule J, et al. Autoimmune hepatitis presenting as acute liver failure: A 20-year retrospective review of North America. Liver Transpl. 2023;29(6):570-580.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.






