A bisbiguanide known as chlorhexidine (CHX) was developed in the UK in the 1940s and has been so
An Insight on Chlorhexidine Use in Dentistry?
ld as a general disinfectant.1 The most effective chemotherapeutic agent and industry standard for decreasing S. mutans and oral biofilm is CHX mouthwash, which is also formulated as toothpaste, gels, chips, and varnishes.
The most successful protocols that deliver the maximum clinical efficacy while minimizing adverse drug reactions are highlighted in a recent study that might assist dentists worldwide with a better understanding of the current applications of chlorhexidine (CHX) in dentistry based on its mechanism of action.
How was the research conducted?
To determine the mechanism of action (MOA) and look into the best supplementary uses of CHX in dental operations, the researchers reviewed the literature. In addition to dentistry textbooks that were obtained from the National Dental Examination Board as well as the University of Toronto Library, databases in the University of Toronto library system were searched for pertinent peer-reviewed articles written in English and published in the previous 5 years. A total of 1100 papers were found, and after reading their abstracts, a total of 100 of them were investigated.
What did they find out about CHX?
This review was specifically focused on CHX mouthwashes because, after a thorough analysis of the articles by the researchers, it was determined that CHX mouthwash is the most effective out of the CHX products due to its ability to successfully inhibit significantly more plaque when compared with gels, varnishes, and other of its formulation.
How does the CHX work?
The extracellular polysaccharides and glycoproteins, phosphate- and sulfate-group-containing bacteria, and other negatively charged locations within the biofilm form a bond with the cationic characteristics of CHX, causing selective and potent adsorption to the surface of the bacterial cell. By passively diffusing through the bacterial cell wall and attacking the cell’s cytoplasmic membrane, this cation damages and compromises the integrity of the cell. This situation enables CHX to penetrate the bacterial cell’s inner membrane, causing the cell’s irreparable damage.
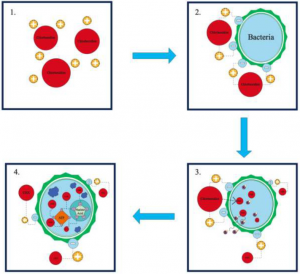
Fig. 1: MOA explained of CHX
The antibacterial effect of CHX is still in the bacteriostatic stage at this time, but it can be reversed by reducing or eliminating CHX. A bacteriocidal stage will develop if the concentration of CHX rises over time or is maintained for a prolonged period and causes irreversible cell damage, showing the bacteriocidal stage. The production of phosphorylated substances, such as adenosine triphosphate and nucleic acids, causes cytoplasmic coagulation and precipitation during the bacteriocidal stage. Due to the negative charge of most oral surfaces (including mucous membranes, teeth, and salivary glycoproteins), CHX has displayed remarkable substantivity of up to 12 hours.
Where can it be used in dentistry?
Products containing CHX can be used therapeutically or preventatively. To make a significant impact while minimizing side effects, CHX is applied at a dose of 18 to 20 mg.
|
Chlorhexidine usage |
Evidence-based recommendations |
| Presurgical | Utilise 0.12% or 0.2% CHX preoperative rinse for 1 minute to reduce oral microbial load prior to implant placement. |
| Postoperative (short-term maintenance) | If toothbrushing is not possible due to postoperative pain, it is recommended that a 0.12% to 0.2% 1-minute rinse is performed 3 times a day for 7 days or until sutures are removed and oral hygiene in the form of toothbrushing can resume. |
| Postoperative (long-term maintenance) | Locally administered sustained-release CHX, in the form of CHX chips, may be considered for use as an adjunct to nonsurgical treatment of peri-implant mucositis and peri-implantitis. Specifically, the use of PeriochipTM over a maximum of 6 months has been suggested in the reduction of implant pocket depth, with a minimum of 2-week recalls. |
Table 1: uses of CHX in dentistry
CHX has quick-acting antibacterial and antifungal properties. It can kill DNA and RNA viruses such the CMV, herpes simplex, hepatitis B, influenza A, parainfluenza, and human immunodeficiency viruses as well as aerobic and anaerobic bacteria.
Dental caries and oral hygiene
CHX mouthwashes have shown considerable reductions in the S. mutans that cause dental caries, but this is not the case for CHX gels and varnish, which did not reduce S. mutans when applied to tooth surfaces. Even though CHX mouthwashes have shown a substantial reduction in S. mutans, this did not indicate any clinically significant decreases in caries.
It is currently possible to combine Chlorhexidine mouthwash with NaF without losing any of the CHX’s anti-plaque, anti-gingivitis, and even anti-S. mutans effects; however, it is not yet known whether CHX impacts fluoride’s qualities, which calls for more research.
When used daily for two weeks without mechanical cleaning, CHX mouthwash with a concentration of 0.1 percent to 0.2 percent exhibits significant antiplaque effects. However, some studies found no differences and others found a considerably reduced antiplaque action with CHX concentrations below 0.12 percent.
Some toothpaste ingredients, such as calcium and anionic surfactants like sodium lauryl sulfate (SLS), can reduce the substantivity and overall effectiveness of CHX and so, to avoid these interactions, CHX mouthwash should be used at least 30 minutes after brushing if it is to be used as an adjunct in oral hygiene.
Periodontal disease
According to numerous studies, Chlorhexidine mouthwash has strong anti-inflammatory and antiplaque effects on the gingiva and teeth when used in concentrations between 0.1 percent and 0.2 percent. However, CHX mouthwash is most effective at 0.12 percent in preventing the growth of gingivitis on a tooth surface free of plaque, so to get a more effective result, patients’ teeth should be cleaned well professionally before its use.
The idea of local delivery of antibacterial agents into periodontal pockets was developed since CHX mouthwash couldn’t reach deep pockets. It has a lower-dose administration at the site of action (the periodontal pocket) sustained over a longer length of time. This was evident when 2.5 mg of CHX gluconate was administered locally using biodegradable CHX “chips” known as Periochip.
Prophylactic use and post–oral surgery procedures
Due to trauma and discomfort following dental surgery, mechanical oral hygiene maintenance may become challenging or even impossible. As a result, after periodontal or implant surgery, CHX mouthwashes are frequently prescribed for a period of 2 weeks and at concentrations between 0.1 percent and 0.2 percent.
After using mouthwash containing 0.12 percent to 0.2 percent CHX, a systemic review revealed a decrease in plaque and halitosis; all trials indicated considerably less plaque buildup in the CHX rinse groups compared to the control groups.
Can CHX cause any adverse reactions (ADRs)?
Even at low concentrations between 0.06 percent and 0.2 percent that are within the therapeutic range, prolonged use of CHX mouthwash may cause the following ADRs:
- Xerostomia, subjective discoloration, altered taste, numbness in the mouth and tongue, and discomfort in the mouth and tongue.
- Long-term usage of CHX mouthwash might result in extrinsic tooth staining and tongue discoloration.
- Some uncommon adverse effects include desquamation of the oral mucosa, parotid gland enlargement, and oral paraesthesia glossodynia.
- Antimicrobial resistance (AMR), a significant adverse effect, is brought on by chronic low-level exposure to CHX.
- Type I and type IV hypersensitivity reactions followed by severe anaphylaxis, which had an incidence of 0.78 per 100,000 exposures, is the most significant ADR connected to oral CHX use.
What does the future hold for Chlorhexidine use in dentistry?
When mechanical prophylaxis is not an option, Chlorhexidine has proven to be an incredibly effective antibacterial in the field of dentistry. Its versatility as a chemotherapeutic agent is unmatched. In periodontics, as a prophylactic, and as an addition to oral health, CHX has shown beneficial effects. The most favorable for long-term usage as an addition to oral hygiene in patients is locally delivered and sustained CHX in the form of CHX chips, it has also significantly aided in a variety of oral surgical procedures, including involvement in implantology and periodontology.
Chlorhexidine mouthwash is preferred over gels and dentifrices due to much superior plaque inhibition with no serious adverse effects hence, as long as the patient does not have a CHX allergy, doctors should not be discouraged from advising CHX mouthwash when required.
References:
- https://pubmed.ncbi.nlm.nih.gov/30888120/
- https://www.cureus.com/articles/19675-comparative-evaluation-of-cocoa-bean-husk-ginger-and-chlorhexidine-mouth-washes-in-the-reduction-of-steptococcus-mutans-and-lactobacillus-count-in-saliva-a-randomized-controlled-trial
- https://www.cdha.ca/pdfs/Profession/Resources/TherapeuticOralRinsingPartI.pdf

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.






