On the occasion of National Toothache Day, we aim to bring attention to the idea that the importance of toothache or teeth pain goes beyond mere discomfort, potentially indicating more profound health issues such as autoimmune conditions. Beyond localized pain, teeth pain emphasizes the need for a comprehensive healthcare approach encompassing dental and systemic well-being.
The impact of autoimmune diseases, affecting approximately 23.5 million Americans, extends to oral health through the inflammation they induce.

Recognizing the intricate link between autoimmune disease and teeth pain prompts a paradigm shift for healthcare practitioners. Encouraging a holistic viewpoint entails addressing immediate dental concerns while acknowledging potential underlying autoimmune conditions. This comprehensive approach, when embraced by physicians, sets the stage for more effective and integrated healthcare, recognizing the interconnected nature of the body’s various systems.
Read this blog to learn about the intricate connection between autoimmune disease and teeth pain, unveiling a physician’s roadmap for providing comprehensive care.
AUTOIMMUNE DISEASE AND TEETH PAIN – UNTANGLING THE CONNECTION
Recent strides in research have illuminated the intricate relationship between autoimmune disease and teeth pain, transcending the conventional boundaries of medical and dental domains. Conditions such as Rheumatoid Arthritis, Systemic Lupus Erythematosus, Pemphigus Vulgaris and Sjögren’s syndrome, traditionally associated with systemic implications, unveil their distinctive manifestations within the oral cavity. This revelation extends beyond the immediate concern of tooth-related issues, encompassing nuanced symptoms like heightened tooth sensitivity, inflammation and, in severe cases, tooth loss.

Please Note: A recent study, as per the National Library of Medicine, delved into oral manifestations of autoimmune diseases. The results indicated that among 50 patients diagnosed with autoimmune conditions, those in the autoimmune disease group had notably higher plaque indexes. Specifically, 70% of cases displayed values equal to or above the median (≥median 35), compared to 54% below the median (˂median 872), with a significant p-value of 0.030.
Once perceived as a compartmentalized aspect of healthcare, the oral cavity emerges as a dynamic diagnostic arena offering profound insights into an individual’s overall health. Dentists and physicians assume pivotal roles in this paradigm, recognizing the early signs within the oral cavity as crucial indicators of potential autoimmune complexities. This collaboration between dental and medical professionals becomes indispensable for achieving a comprehensive understanding and nuanced management of these conditions.
Recognizing these early indicators not only expedites the diagnosis and intervention of autoimmune disorders but also accentuates the significance of a cohesive healthcare approach. Through synergistic collaboration, dentists and physicians can craft a unified care plan that adeptly addresses both the immediate oral health concerns and the broader autoimmune landscape. This approach ensures a holistic and advanced standard of patient care that acknowledges the intricate interplay between autoimmune disease and teeth pain.
DECIPHERING AUTOIMMUNE ONSLAUGHT ON ORAL HEALTH
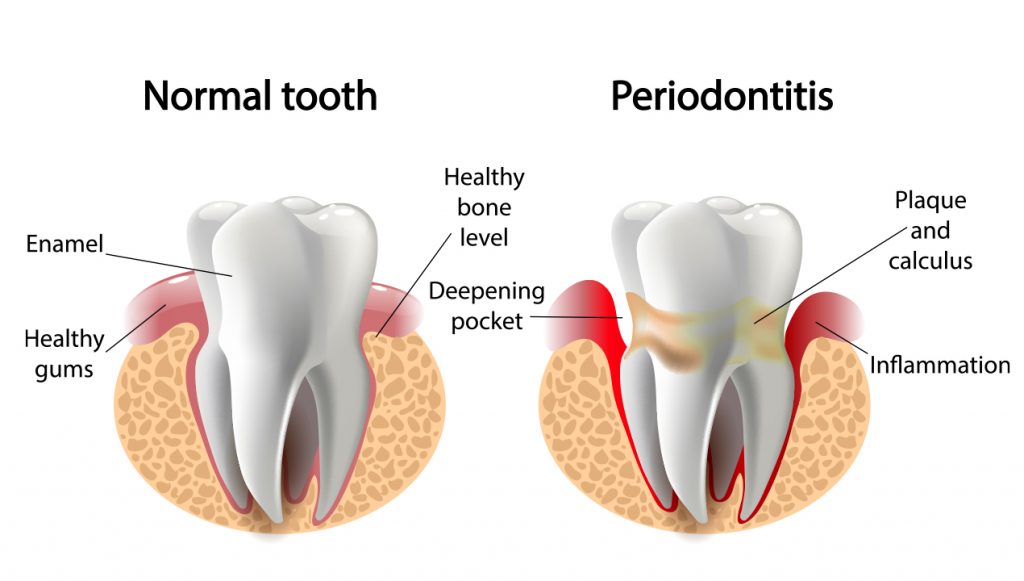
Autoimmune ailments unfold as the immune system erroneously targets and attacks healthy cells and tissues. This complicated interrelation between the body’s defenses and constituents extends its impact on oral health, precipitating conditions such as periodontitis. In this autoimmune-driven scenario, the immune response strategically targets the tissues surrounding the teeth. Consequently, patients contend with persistent toothaches, bleeding gums and an array of other oral health issues.
Understanding the complexities of this immune response within the oral cavity is pivotal in comprehending the broader implications for patients suffering from autoimmune complexities.
The delicate balance between the immune system and oral health highlights the imperative for a holistic healthcare approach that integrates the systemic immune response with immediate dental concerns. This awareness facilitates early detection and guides healthcare practitioners in devising comprehensive care plans that navigate the intricate terrain between the body’s defenses and the well-being of oral tissues.
PHYSICIAN’S GUIDE TO HOLISTIC CARE: A COMPREHENSIVE ROADMAP
When addressing autoimmune disease and teeth pain, physicians should adopt a meticulously designed plan, such as the one outlined below. This approach ensures comprehensive and tailored care to enhance patient outcomes:
- Collaborate with Dentists
Physicians and dentists are essential collaborators in meticulously managing autoimmune ailments, seamlessly addressing both the oral and systemic dimensions.
The cultivation of consistent and robust communication between these healthcare professionals is paramount, ensuring the precision of diagnoses and the development of comprehensive treatment plans tailored to individual patient needs. This synergistic approach guarantees a heightened standard of care for those navigating the complexities of autoimmune disease and teeth pain.
- Give Importance to Early Detection & Diagnosis
The discernment of signs indicative of autoimmune disorders within the oral cavity is paramount for early intervention. Physicians ought to undergo training that equips them with the ability to identify oral manifestations of autoimmune diseases during routine check-ups.
This proficiency prompts a subsequent and thorough investigation into potential autoimmune connections, ensuring a proactive approach to patient care and comprehensive health management.
- Personalize Treatment Plans
The uniqueness of each patient’s presentation of autoimmune conditions highlights the need for a customized treatment strategy. A personalized plan, essential in its design, meticulously addresses the dental and systemic facets of their health.
This tailored approach may involve a thoughtfully curated blend of medications, lifestyle adjustments and precise dental interventions, culminating in a comprehensive and effective healthcare regimen tailored to the individual nuances of the patient’s condition.
- Educate the Patients

Providing patients with comprehensive education regarding the correlation between autoimmune disease and teeth pain is paramount. Empowered individuals are more inclined to proactively engage in their healthcare journey and adhere to prescribed treatments, cultivating improved long-term outcomes.
- Take a Multidisciplinary Approach
Enlisting a multidisciplinary approach that integrates the expertise of rheumatologists, dentists and other specialized professionals is instrumental in formulating a comprehensive strategy for the management of autoimmune disease and teeth pain. This collaborative effort fosters a more nuanced and holistic perspective on the patient’s health, considering both the systemic and oral dimensions.
Rheumatologists contribute their expertise in understanding and treating autoimmune disorders from a systemic standpoint, providing insights into the broader health implications. Dentists, equipped with a deep understanding of oral health intricacies, offer valuable perspectives on how autoimmune conditions may manifest within the oral cavity.
The collaboration extends beyond these core disciplines, incorporating other specialists as needed, ensuring a well-rounded and inclusive approach. This collective effort enables a thorough examination of the patient’s health, taking into account the link between autoimmune disease and teeth pain.
CONCLUSION

Physicians stand at the forefront as architects of exceptional care, adeptly navigating the link between autoimmune disease and teeth pain. Their proactive and meticulously crafted approach, bolstered by early detection and seamless collaboration with dental experts, epitomizes the essence of the strategic blueprint for tackling these health complexities.
This dynamic orchestration ensures effective treatment and promises a transformative and impactful experience for individuals grappling with the intricate nuances of autoimmune disease and teeth pain.
Physicians reading this blog, we invite you to join MDForLives, a platform tailored for sharing your distinctive viewpoint via paid medical surveys, articles and case studies. Upon becoming a member, you will also get access to our webinars and discussion forums.
References:
- Poor Oral Health Associates with Incidence of Autoimmune Diseases
www.ncbi.nlm.nih.gov
- Oral Signs Are Frequently the First Manifestation of Autoimmune Diseases
www.hindawi.com - 23.5 million Americans living with an autoimmune disease, the associated inflammation they cause is affecting our oral health
www.dhconcepts.com - Autoimmune Diseases and Their Manifestations on Oral Cavity: Diagnosis and Clinical Management
www.ncbi.nlm.nih.gov

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.



