For several years we have approached a ‘standard of care’ (SOC) for the treatment of metastatic HER2-positive breast cancer. In the first-line setting, we have been treating with the THP regimen (docetaxel, trastuzumab, and pertuzumab. Also called Taxotere), in accordance with the CLEOPATRA Study. This study was recently updated with almost 100 months of follow-up, with immediate OS (overall survival) observed in favor of pertuzumab (57.1months vs 40.8months placebo).
Following this, the results of the EMELIA study led to a SOC in the second line. This was a study looking at T-DM1 (trastuzumab emtansine) with an OS benefit of 29.9m vs 25.9 with capecitabine + lapatinib and a hazard ratio of 0.75.
However, what of the third line and beyond?
Over the last 2 years, a number of novel treatments have emerged that look to address this unmet need.
We have 2 oral HER2 TKIs (tyrosine kinase inhibitors): Neratinib (approved by the FDA in February 2020), and Tucatinib (approved in April 2020).
We have 2 HER2 ADCs (antibody-drug conjugates): Trastuzumab deruxtecan (T-DXd; approved in December 2019), and Trastuzumab duocarmazine/Trastuzumab-vc-seco-DUBA (SYD985).
We also have re-engineered HER2 Mab (monoclonal antibodies): Margetuximab (approved in December 2020).
Neratinib
In certain subsets of brain metastases, CNS (central nervous system) progression-free survival was markedly improved.
The evidence of the NALA study shows there is a role for neratinib in CNS metastases. Indeed, amongst 3 patients with LMD (Leptomeningeal disease) in the neratinib arm, 2 patients had PFS of 5.6 and 9.8m with OS of 17.4 and 19.8, compared to the lapatinib arm, where 1 patient had progressed at 4.3m with OS of 6.5m.
Tucatinib
In the phase II HER2 CLIMB study, tucatinib combination (tucatinib + trastuzumab + capecitabine) vs comparator arm (placebo + trastuzumab + capecitabine), the enrolment criteria are listed below:
The results demonstrated an improvement in mPFS of 7.8m tucatinib vs 5.6m placebo, with a 41% ORR (objective response rate) for tucatinib combo vs 23%. The OS graph below shows a significant improvement in mOS.
On 17 April 2020, based on these good results, te FDA approved tucatinib combination for HER2-positive metastatic breast cancer after prior therapy with an anti-HER2 drug.
Trastuzumab Deruxtecan
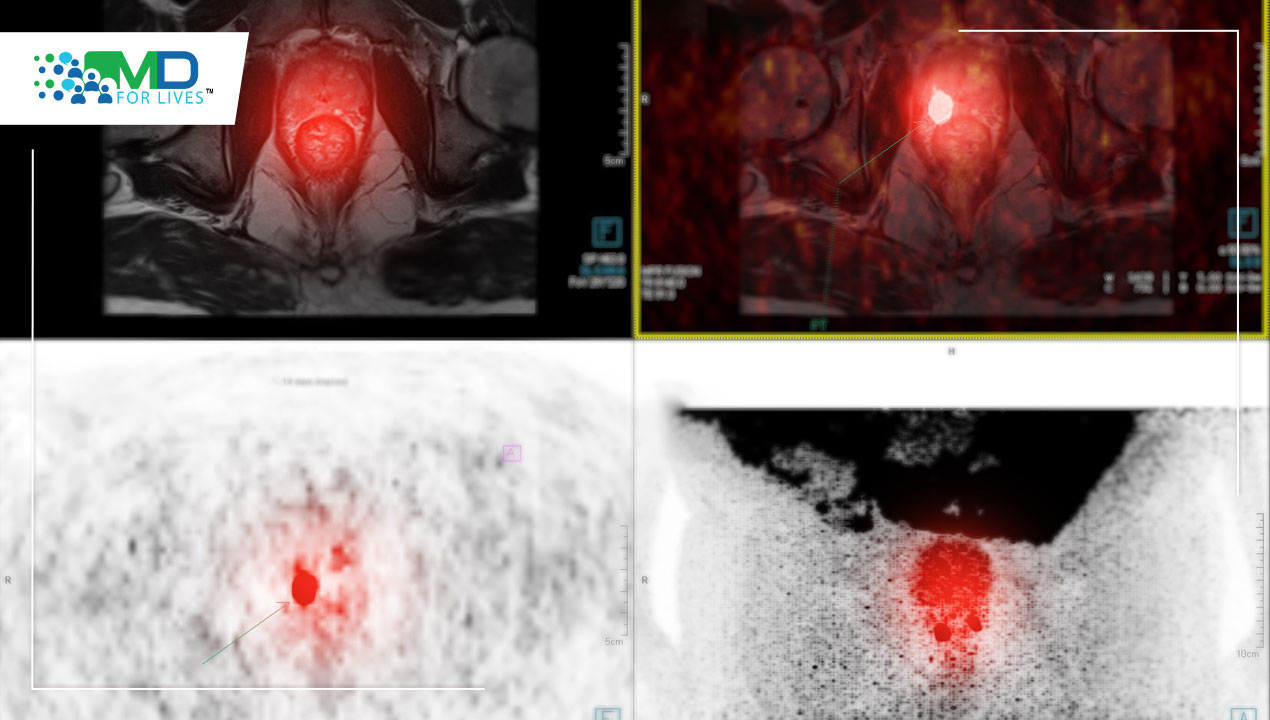
T-DXd was evaluated in the DESTINY-Breast01 trial.
Below is the waterfall plot, which shows an impressive 60.9% ORR.
The mPFS after 11.1 months was 16.4m, and 18.1m in those patients with brain metastases
After 20 months, mPFS rose to 19.4m, with a mOS of 24.6m (though only 35% of events were captured). Though cross-study analysis is discouraged, the results of DESTINY-Breast01 showed an improvement of D-DXd compared to THP used in the CLEOPATRA trial.
Below shows the initial presentation head to head with the June 2020 presentation, showing considerable improvements in DOR (duration of response) and PFS.
The data below shows consistent objective response from the 2nd line to the 6th line. There were no differences in ORR by any of the subgroups that were interrogated.
The toxicities are shown below, with very few Grade 3 side effects:
Though Grade 4 and 5 events of interstitial lung disease were observed:
As a result, the following algorithm was recommended by the sponsor:
TDX-d + Nivolumab
There has been another study of T-DXd with the anti-PD-1 antibody nivolumab, which has shown a promising anti-tumor effect
The encouraging waterfall plot below shows good efficacy in both HER2 positive and HER2 Low cohorts, in those that had up to 5 prior treatments.
TDX-d vs T-DM1 IN 2nd Line
The Destiny-Breast03 study is underway, with results expected in Feb 2022, and could possibly shift the standard of care from T-DM1 to T-DXd in second line.
HER2-Targeted ADC: Trastuzumab Duocarmazine (SYD985)
Trastuzumab duocarmazine is a HER2 antibody with the same amino acid sequence as trastuzumab. The proteolytic cleavage of linker in tumor microenvironment leads to the activation of the prodrug payload. It has an active toxin (DUBA) that alkylates DNA, killing dividing and non-dividing cells. Like other ADCs, it has a bystander-killing effect.
In a phase I study, the waterfall plot showed an ORR of 33%, with mild to moderate toxicities, and conjunctivitis, dry eye, and increased lacrimation most common reasons for discontinuation.
Margetuximab
The SOPHIA study shows Margetuximab vs Trastuzumab in HER2+ advanced BC after 2 or more HER2 therapies.
There were 2 analyses, a year apart showing slight improvement in PFS compared to the trastuzumab arm.
OS again had a slight improvement, but we shall find out more from this study this year.
HER2 sequencing
With the numerous advances in HER2+ treatment options, how do we best sequence regimens? The table below gives a possible option.
The Future
There have been a number of advances in PI3K inhibitors, CDK4/6 inhibitors, and checkpoint inhibitors, plus we are waiting on trial data re: Margetuximab and Pyrotinib (an irreversible dual pan-ErbB receptor tyrosine kinase inhibitor).
With such an array of trials and treatments, the landscape of HER2-positive breast cancer looks bright and in bloom.