According to the World Health Organization (WHO), it is estimated that 1 out of 700 newborn babies are born with oral clefts, and the condition varies in each case [3]. It is the most common facial anomaly among live births. During the 4th and 10th week of the developing embryo or fetus, a gap or split in the lip and/or the palate (roof) of the mouth can be formed due to the interruption of embryonic growth between (Peterson-Falzone, Hardin-Jones, & Karnell, 2010) [1]. This is known as a cleft lip, cleft palate or both. Oral clefts that are physically examined by an ENT doctor or attending physician can easily classify the cleft from mild to severe or the laterality on the sides of the mouth.
Since clefting has visible physical changes, a cleft palate or cleft lip is easy to diagnose. According to the Cleft Registry and Audit NEtwork (CRANE) Database based in the United Kingdom, around 81% of cases can be determined using prenatal ultrasound. If a cleft has not been detected in an ultrasound prior to the baby’s birth, a physical inspection of the mouth, nose and palate after live birth confirms the presence of cleft lip or cleft palate.
In most cases, the cause of oral clefts are unknown. A multifactor inheritance or the correlation between genes within the family is one of the leading causative theories by scientists of today. [4] Chromosomal differences and genetic mutations can induce clefting in syndromes. Since most syndromes have malformations as an indicator, an amniocentesis test (where a sample of the fluid surrounding the developing baby is taken and analysed) is attempted to detect syndromes with the potentially greater impact such Edwards and Down’s syndrome [6]. Even though studies have yet to prove the direct link of environmental risk factors, epidemiological and experimental data suggest that maternal exposure to tobacco smoke, alcohol, poor nutrition, viral infection, medicinal drugs and teratogens in the workplace and at home in early pregnancy should be noted by the attending physician. Folic acid is mostly prescribed to prevent most congenital disabilities. Although oral clefts are not totally preventable, pregnant mothers are partnered with a preconception counsellor who can guide and ensure maternal health.
Other Associated Conditions
The first thing that comes to mind would be difficulty in feeding, swallowing and mechanisms of the mouth. Foods and liquids can pass to the nose from the opening of the palate in the mouth. Children with a cleft palate would be advised to wear a human-made palate to ensure that that they acquire adequate nutrition before they undergo on reconstructive surgery. Compared with peers of the same age, children with cleft lip and palate have developmental delays in speech and language. Dental and orthodontic problems are common as well due to the malformation, absence or displacement of teeth.
Breathing is relatively normal in patients, but resonance and airflow may be compromised, causing hypernasality (excessive resonance in the nasal cavity when producing vowel sounds) and nasal air emission. Children with unrepaired cleft palate can acquire middle ear problems such as ear infection and Eustachian tube dysfunction, which if untreated, lead to conductive hearing loss. Though not fatal to the infant’s health, adverse effects on speech, hearing, appearance, and psychology can lead to a delay in development and social integration.
Growing up: Treatment and Management
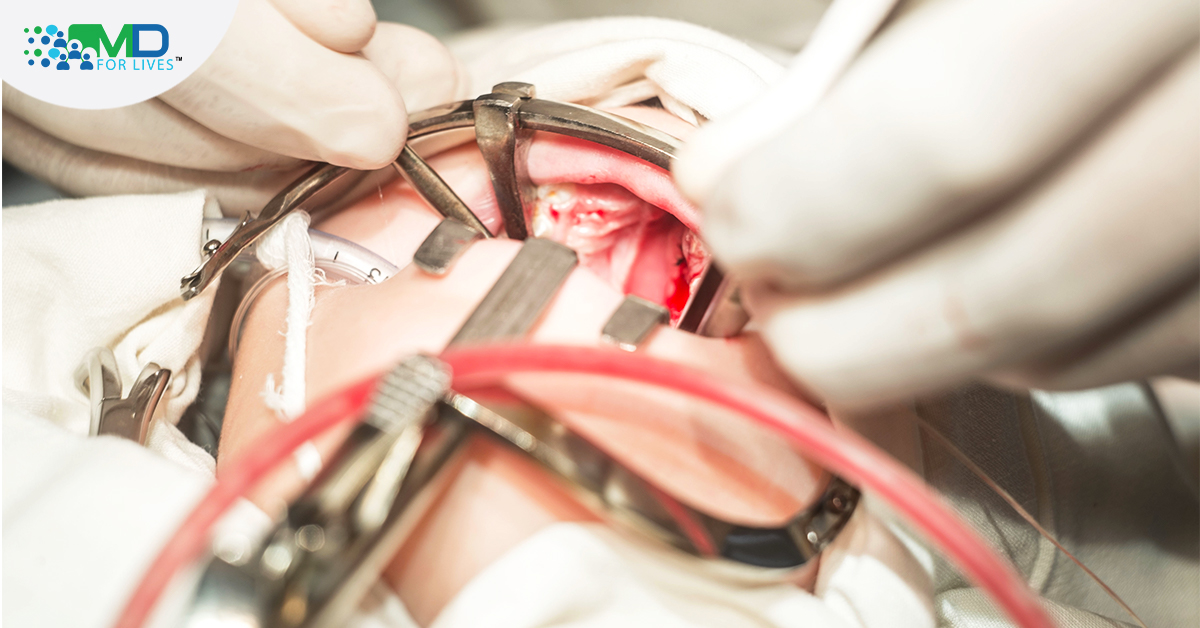
Treatment for children with oral clefts requires rehabilitation and consistent care from a team of health professionals until adulthood. The cleft palate team should mainly include a surgeon who specialises in cleft surgical management, a speech pathologist and a dental professional. Often than not, children with clefts require a number of surgeries, along with long-term follow-ups. Surgery to repair a cleft lip is usually done between 10 to 12 weeks of age. The cleft palate repair procedure, called “palatoplasty,” is done between nine and 18 months [2]. This helps improve speech and prevents the food and liquids from leaking out of the nose. [7]
Outside the cleft management team, other health professionals such as paediatricians, audiologists, geneticists and psychologists can be consulted by the parents for further management. Discussing treatment options can help put your mind at ease and decide what you want for your child’s future. Speech defects, hearing loss, feeding problems and psychosocial issues can all be improved by the cleft treatment pathway laid by the cleft team. Children with clefts should be thought of as, with few exceptions, normal children who happen to have been born with a congenital disability. Parents, family relatives and teachers of children with clefts should be informed and encouraged to learn as much as they can about oral clefts and then to teach people that surround them about what they learned [5]. With proper parental guidance combined with a multidisciplinary approach from the medical team, children born with a cleft lip and palate have the most exceptional care.

REFERENCES
[1] American Cleft Palate-Craniofacial Association. (2009). Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Chapel Hill, NC: Author.
[2] American Academy of Otolaryngology–Head and Neck Surgery Foundation. (2019). https//www.enthealth.org/conditions/cleft-palate/
[3] American Speech-Language-Hearing Association. (2016). Scope of practice in speech-language pathology
[4] Dixon, Michael J., et al. “Cleft lip and palate: understanding genetic and environmental influences.” Nature Reviews Genetics 12.3 (2011): 167-178.
[5] Karnell, M. Cleft palate: Frequently Asked Questions. (2012). https//uichildrens.org/health-library/cleft-palate-frequently-asked-questions
[6] Murray, J. C. “Gene/environment causes of cleft lip and/or palate.” Clinical genetics 61.4 (2002): 248-256.
[7] Kellog, B., et.al. “Cleft Palate for Parents”. (2019). https//kidshealth.org/en/parents/cleft-palate.html