Ectopia lentis is an ophthalmic condition characterized by displacement or malposition of the crystalline lens from its normal anatomical location. This displacement disrupts the eye’s refractive mechanism and can lead to significant visual impairment if not properly managed. It may present as an isolated ocular condition or as part of a broader systemic or genetic disorder, making early diagnosis and comprehensive evaluation essential.
This article provides an in-depth overview of Ectopia Lentis, including its causes, clinical features, associated ocular and systemic conditions, diagnostic approach, radiological findings, management strategies, and insights from recent studies. A real-world pediatric case is also discussed to highlight practical clinical considerations.
What Is Ectopia Lentis?
Ectopia lentis refers to partial or complete displacement of the crystalline lens due to weakened, damaged, or absent zonular fibers. The lens may shift superiorly, inferiorly, nasally, or temporally depending on the underlying etiology.
How Does Ectopia Lentis Affect Vision?
Lens displacement interferes with proper focusing of light onto the retina, resulting in:
- Blurred or fluctuating vision
- High refractive errors
- Irregular astigmatism
- Reduced visual acuity
In pediatric patients, if left untreated it may lead to amblyopia and permanent visual impairment.
Who is Affected by Ectopia Lentis?
It can occur in:
- Children with congenital or genetic causes
- Adolescents and adults with acquired or traumatic causes
Pediatric cases pose additional challenges due to ocular growth, neurodevelopmental factors, and limited compliance with optical correction.
Ectopia Lentis: Symptoms and Causes
Common Symptoms
- Blurred vision
- Decreased visual acuity
- Monocular diplopia
- Refractive errors such as myopia, hyperopia, or astigmatism
- Visible lens edge on slit-lamp examination
Causes of Ectopia Lentis
It may result from:
- Genetic connective tissue disorders
- Metabolic abnormalities
- Ocular trauma
- Degenerative weakening of zonular fibers
Ectopia Lentis as a Disease Entity
Ocular Diseases Associated With it
- High myopia
- Refractive amblyopia
- Secondary glaucoma
- Retinal detachment
Other Ocular Disorders Associated With it
- Lens-induced uveitis
- Cataract formation
- Irregular pupil configuration
Systemic Diseases Associated With it
- Marfan syndrome
- Homocystinuria
- Weill–Marchesani syndrome
Other Systemic Associations
- Ehlers–Danlos syndrome
- Sulfite oxidase deficiency
- Hyperlysinemia
Identifying systemic associations is critical, as ectopia lentis may be the first clinical manifestation of an underlying genetic or metabolic condition.
Ectopia Lentis Diagnosis
Accurate diagnosis relies on clinical evaluation combined with imaging and systemic assessment.
History
- Age at onset
- Family history of connective tissue or metabolic disorders
- History of ocular trauma
- Presence of developmental delays or systemic symptoms
Physical Examination
- Slit-lamp examination to assess lens position
- Evaluation of zonular integrity
- Measurement of intraocular pressure
Laboratory Tests
- Plasma homocysteine levels when homocystinuria is suspected
- Genetic testing in selected cases
Differential Diagnosis
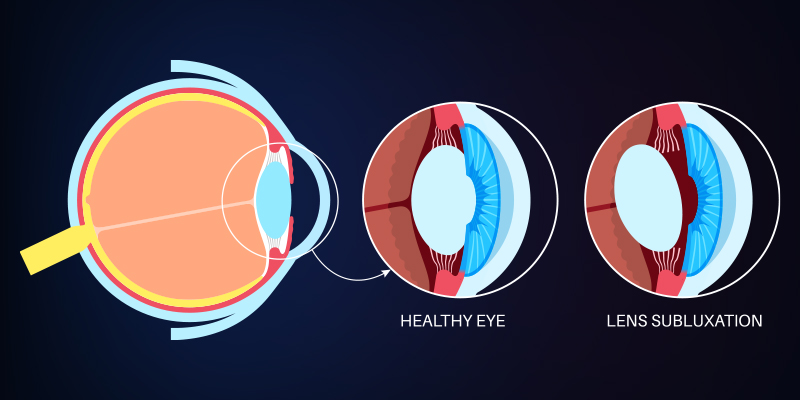
Diagram illustrating Ectopia Lentis with lens subluxation
- Traumatic lens dislocation
- Intraocular lens displacement in pseudophakia
- Lens subluxation secondary to chronic uveitis
Radiological Features
Ultrasound (B-scan)
- Useful when media opacity limits direct visualization
- Confirms lens displacement in pediatric or uncooperative patients
CT Imaging
- Demonstrates lens location in cases of complete dislocation
- Helps identify associated ocular or orbital trauma
Radiological imaging is particularly valuable when clinical examination is inconclusive.
Management and Treatment of Ectopia Lentis
Management depends on the degree of lens displacement, visual impairment, patient age, and associated ocular or systemic conditions.
Medical Management
- Optical correction using spectacles or contact lenses
- Amblyopia therapy in children
- Regular monitoring when lens displacement is mild and vision is stable
Surgical Management
Surgical intervention is indicated when:
- Visual acuity cannot be adequately corrected
- Progressive lens displacement is observed
- Secondary complications such as glaucoma develop
Surgical options include:
- Lens extraction
- Capsular tension devices
- Scleral fixation techniques
- Intraocular lens implantation
Real-World Clinical Considerations
In real-world practice, ectopia lentis is often diagnosed later than ideal, particularly in pediatric patients with developmental delays or limited ability to communicate visual symptoms. Early signs may be subtle, refractive changes may be attributed to routine pediatric ametropia, and follow-up is frequently inconsistent.
Beyond diagnosis, clinicians often face challenges related to long-term monitoring, access to specialized surgical expertise, and variability in caregiver adherence to optical correction and amblyopia therapy. In many cases, outcomes are shaped as much by follow-up reliability and compliance as by the surgical technique itself.
These practical constraints highlight why standardized management pathways do not always translate cleanly into real-world pediatric care.
Clinical Perspective: Pediatric Case Context
A pediatric case involving a 7-year-old female with bilateral ectopia lentis, developmental delay, and high anisometropic hyperopic astigmatism illustrates real-world management challenges.
The patient demonstrated poor compliance with spectacle use and significant lens subluxation. Surgical management included capsular tension segment fixation, scleral stabilization using double-flanged polypropylene sutures, and in-the-bag intraocular lens implantation.
Postoperative follow-up showed improved visual acuity and stable lens positioning, highlighting the importance of individualized surgical planning and long-term follow-up in pediatric ectopia lentis.
Clinical Interpretation
This case underscores several real-world challenges that are common in pediatric cases but often underappreciated. Poor spectacle compliance, compounded by developmental delay, significantly limited non-surgical management options. Surgical decision-making was therefore driven not only by anatomical findings, but by the practical inability to achieve visual rehabilitation through conservative means. Long-term follow-up remains critical in such cases, as visual outcomes depend heavily on postoperative monitoring, refractive adjustment, and amblyopia management rather than surgical success alone.
Prognosis and Future Directions
The prognosis of ectopia lentis varies depending on:
- Underlying etiology
- Timeliness of diagnosis
- Adequacy of refractive correction
- Surgical technique and postoperative care
Recent studies focus on improved scleral fixation methods, safer pediatric intraocular lens implantation, and genetic characterization of it. Advances in imaging and surgical technologies continue to refine management strategies..
Why Rare Conditions Like Ectopia Lentis Need Real-World Insight
Rare ophthalmic conditions illustrate the limitations of guideline-only decision-making. Variability in presentation, delayed diagnosis, inconsistent follow-up, and caregiver-dependent compliance often shape outcomes more than textbook management algorithms.
MDForLives enables healthcare professionals to share real-world experiences across such complex care pathways, helping surface practical challenges that are rarely captured in clinical trials. These insights support better understanding of how rare conditions are managed outside controlled settings and where care pathways most often break down.
Frequently Asked Questions
How does homocystinuria cause Ectopia Lentis?
Homocystinuria weakens zonular fibers through metabolic disruption, leading to lens displacement, often in an inferior direction.
Can it cause blindness?
If left untreated, Ectopia Lentis can result in severe visual impairment due to amblyopia, glaucoma, or retinal complications.
What is isolated Ectopia Lentis?
It refers to lens displacement without associated systemic disease.
What is Ectopia Lentis associated with Marfan syndrome?
In Marfan syndrome, it commonly presents as superotemporal lens displacement due to connective tissue weakness.
What is the most common cause of acquired Ectopia Lentis?
Ocular trauma is the most common cause.
How MDForLives Supports Ophthalmology Research
MDForLives enables healthcare professionals to contribute real-world insights through structured surveys and research participation. These insights support better understanding and management of rare and complex ophthalmic conditions such as Ectopia Lentis.

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.


