ABSTRACT
This case study presents a patient with a complex medical history admitted with a prolonged QTc interval on her initial EKG. Unfortunately, this critical detail went unnoticed, leading to a life-threatening arrhythmia known as Torsades de Pointes (TdP), which caused a cardiac arrest.
Long QT syndrome (LQTS) is when the heart takes longer than normal to recharge between beats, a prolonged QT interval on an EKG. This case emphasizes the importance of recognizing Long QT Syndrome symptoms early so patients can be carefully monitored, avoid medications that worsen the condition, and receive timely treatment for electrolyte imbalances.
INTRODUCTION
Long QT Syndrome (LQTS) can be congenital or acquired, with drug therapy being the most common cause of the acquired form. Several factors increase the risk of developing drug-induced Long QT Syndrome, including low potassium or magnesium levels, slow heart rate, certain medical conditions like thyroid or kidney disease, and anorexia.
CASE REPORT
This case involves a 27-year-old woman with a history of Addison’s disease, hypothyroidism, primary ovarian failure, osteoporosis, and a pattern of not consistently following her prescribed treatments.
She initially came to the emergency department with flu-like symptoms and tested positive for COVID-19. Doctors treated her with IV fluids, high-dose steroids, and Paxlovid, stabilizing her for discharge.
About 10 days later, she returned with a fever, muscle pain, fatigue, cough, and difficulty breathing. Upon arrival, she was found to be hypotensive with blood pressure in the 80s, a fever of 103°F, and an elevated white blood cell count. She also had abnormal thyroid levels and ketones in her urine, suggesting some metabolic imbalance. She was treated with fluids, antibiotics, and steroids for a possible urinary tract infection and sepsis.
During her hospital stay, she developed abdominal pain, and tests showed possible gallbladder inflammation. Surgery was deemed necessary, and she underwent a laparoscopic cholecystectomy, which went smoothly. However, the following day, she had several episodes of unresponsiveness, a slow heart rate, and low oxygen levels. She was found to have frequent Premature Ventricular Contractions (PVCs) and eventually developed TdP, a dangerous heart rhythm that led to cardiac arrest.
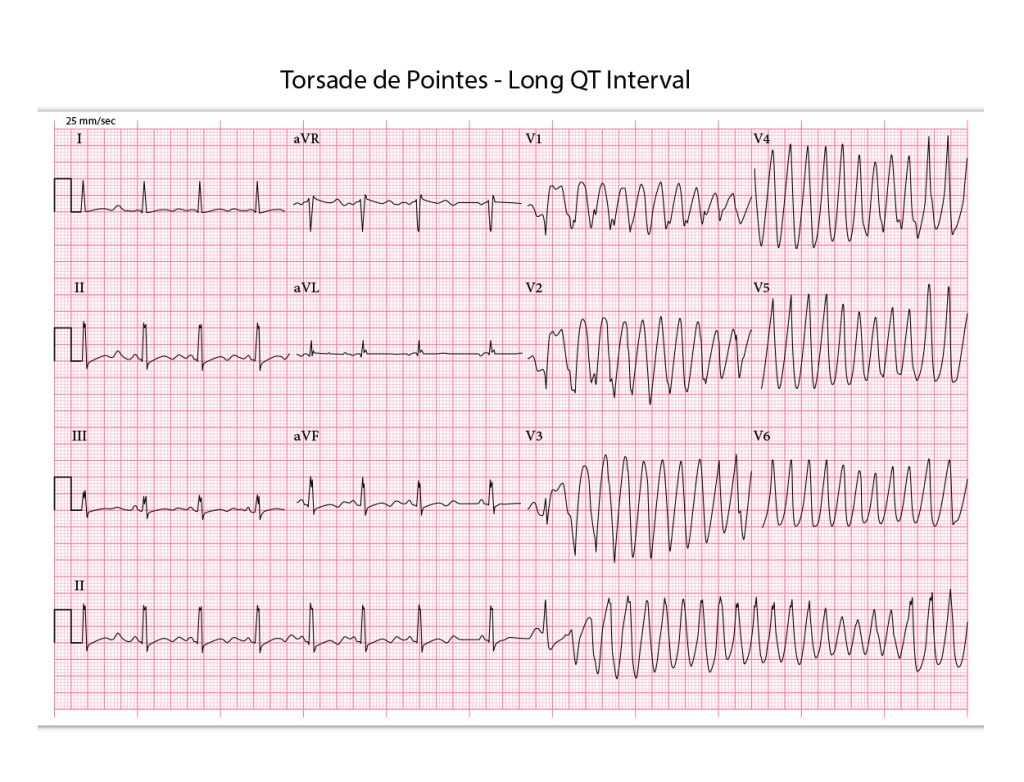
Her blood tests revealed low potassium and calcium, but no magnesium level had been checked earlier. She was treated with magnesium and potassium, and an EKG showed a prolonged QT interval of 593 milliseconds. Upon reviewing her admission EKG, it was found that her QTc had already been prolonged at 549 milliseconds (an overlooked critical sign of Long QT Syndrome). The patient was transferred to intensive care for Long QT Syndrome treatment, where she experienced another brief episode of TdP. She was given emergency treatment, including amiodarone, more magnesium, calcium, and potassium, before being transferred to a higher-level facility. There, she received an Implantable Cardioverter-Defibrillator (ICD) to manage her heart rhythm in the future.
DISCUSSION
This patient’s complex medical history, including Addison’s disease, increased her risk for Long QT Syndrome despite her young age. Fortunately, with proper Long QT Syndrome treatment, she recovered without further complications.
Testing didn’t reveal any genetic or structural causes for her prolonged QTc, but she was treated with Long QT Syndrome medication and supplements to manage her heart condition and electrolyte levels. Her thyroid medication was also adjusted, and she was sent home with instructions to take stress-dose steroids when needed.
CONCLUSION
This case highlights the importance of identifying Long QT Syndrome early, whether congenital or acquired. If the patient’s prolonged QTc had been noticed on her initial EKG, doctors could have monitored her more closely on telemetry. They could have avoided medications like Zofran that prolong the QT interval and replenished her electrolyte levels (especially magnesium, calcium, and potassium) more quickly. Given her history of Addison’s disease and steroid use, these precautions were particularly important. Additionally, an early cardiac consultation might have altered her Long QT Syndrome treatment course, potentially avoiding a dangerous arrhythmia and cardiac arrest.

Dr. Arlene N. Chua graduated from East Carolina University School of Medicine, trained in General Surgery, and later switched to Family Medicine, completing her residency at Virginia Commonwealth University. She has over 20 years of experience in Emergency Medicine.