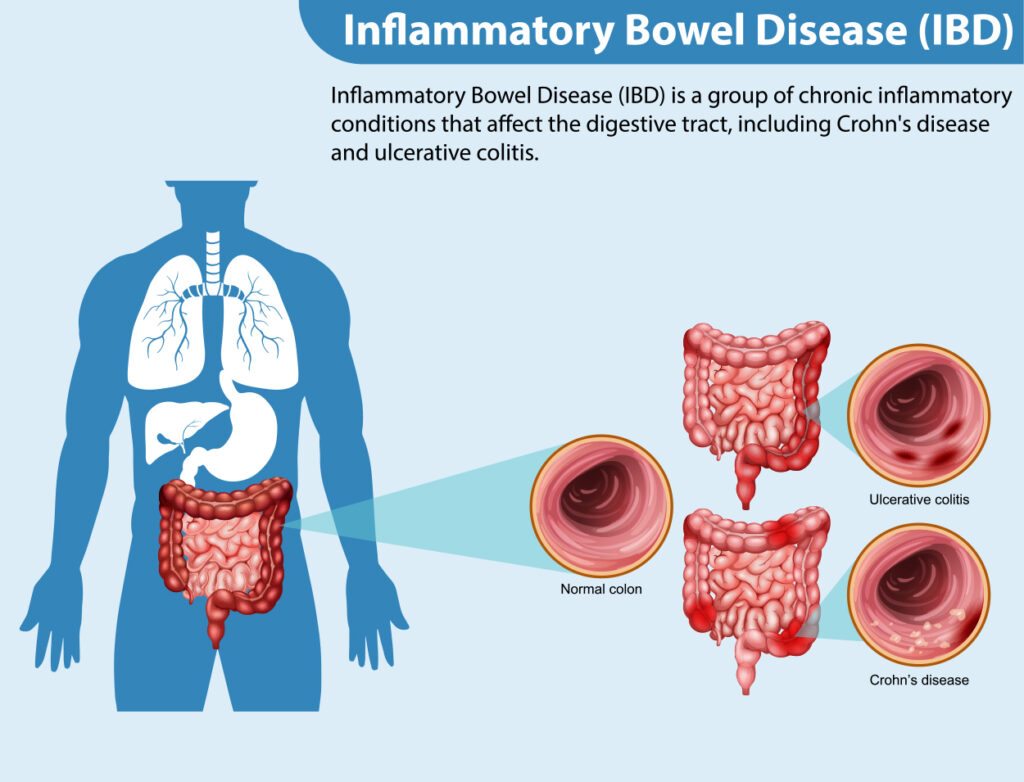
What if the key to managing Inflammatory Bowel Disease (IBD) lies in the trillions of microbes that call our gut – their “home”? These microscopic organisms, known as the ‘gut microbiome,’ are fundamental to our health. They support digestion, regulate immune responses, and maintain a harmonious internal environment. However, in patients with IBD, such as Crohn’s Disease and Ulcerative Colitis, this delicate ecosystem often falls out of balance. This leads to increased inflammation and worsening symptoms.
For years, IBD treatments have primarily focused on suppressing inflammation and relieving symptoms through medications like corticosteroids, immunosuppressants, and biologics. While these approaches have significantly improved patient care, they do not fully address one critical aspect – restoring the gut’s natural harmony. This is where the emerging field of Microbiome-based therapies comes into play.
As we observe Crohn’s and Colitis Awareness Week, it is the perfect opportunity to highlight the groundbreaking Microbiome-based therapies that go beyond the conventional symptom management strategies.
GUT MICROBIOME IMBALANCE: HOW IS IT CONNECTED TO IBD?
The gut microbiome, a complex ecosystem of trillions of microorganisms, is vital for maintaining optimal gastrointestinal health. However, in individuals with Inflammatory Bowel Disease (IBD), this intricate balance is frequently disrupted, leading to a state known as gut dysbiosis, which plays a crucial role in the pathogenesis of IBD.
Research has shown that IBD patients exhibit:
- A significant decline in beneficial bacteria, such as Faecalibacterium prausnitzii, known for its anti-inflammatory effects.Studies have shown that levels of Faecalibacterium prausnitzii can drop by up to 80% in IBD patients compared to healthy individuals.
- An increase in pro-inflammatory bacteria like Bacteroides and Firmicutes, which contribute to the chronic inflammation that defines IBD.Research suggests these bacteria are present in higher concentrations in IBD patients, intensifying the persistent inflammation in conditions such as Crohn’s Disease and Ulcerative Colitis.
These imbalances aggravate symptoms and drive the onset and progression of IBD, making conventional treatments less effective.
A study published in Nature Reviews Gastroenterology & Hepatology found that
IBD patients with severe dysbiosis were 30% less likely to respond to standard treatments.
As researchers delve deeper into these microbial disruptions, they uncover innovative therapeutic approaches that target the root cause of IBD rather than just managing symptoms.
For instance, microbiome-based therapies such as Fecal Microbiota Transplantation (FMT) are being explored as potential treatments, with early trials showing promising results. In fact, a study published in Gastroenterology in 2023 found that FMT led to 50% remission rates in patients with Ulcerative Colitis who did not respond to conventional therapies.
This shift towards microbiome-based treatments offers hope for more personalized and effective IBD care, potentially transforming Crohn’s and ulcerative colitis management.
PROMISING MICROBIOME-BASED THERAPIES ON THE HORIZON
Microbiome-based interventions focus on rebalancing gut bacteria, reducing inflammation, and improving overall gut health.
Here are the three key microbiome-based therapies for inflammatory bowel disease that are gaining traction:
1. Fecal Microbiota Transplantation (FMT)
FMT involves transplanting stool from a healthy donor to an IBD patient, to restore gut microbiome. While still under investigation for Crohn’s and ulcerative colitis, early results show promise in reducing symptoms and inducing remission.
2. Probiotics, Prebiotics and Synbiotics
- Probiotics introduce beneficial bacteria, such as Lactobacillus and Bifidobacterium.
- Prebiotics promote the growth of these beneficial microbes by supplying essential nutrients.
- Synbiotics combine the two, amplifying their synergistic effects.
3. Microbial Metabolite Therapies
These therapies focus on restoring important substances in the gut, such as short-chain fatty acids (SCFAs), produced by gut bacteria when they break down dietary fiber.
SCFAs, including acetate, propionate, and butyrate, help maintain a healthy gut and have anti-inflammatory effects. They are vital in keeping the gut lining strong and reducing inflammation, especially for people with Inflammatory Bowel Disease (IBD).
Please note: A study published in Cell Host & Microbe (2019) demonstrated that increasing SCFAs through Fecal Microbiota Transplantation (FMT) significantly reduced inflammation by up to 50% in patients with inflammatory bowel disease (IBD).
COMBINING MICROBIOME THERAPIES WITH TRADITIONAL APPROACHES – MUCH NEEDED!
While microbiome-based therapies for inflammatory bowel disease have shown great promise, they are not intended to replace traditional approaches. Instead, these therapies can interact constructively with existing treatments like – biologics, immunosuppressants, and anti-inflammatory medications.
For instance, in refractory IBD cases, where conventional therapies may fall short, combining Fecal Microbiota Transplantation (FMT) with biologics has shown improved outcomes!
FMT works by reintroducing a diverse range of beneficial bacteria, helping to restore gut microbiome and reduce inflammations. When paired with biologics, which target specific immune pathways to regulate inflammation, this combination therapy can enhance therapeutic efficacy, improving symptom control, reducing flare frequency, and slowing disease progression.
Beyond FMT, probiotics and dietary interventions are also being explored alongside traditional therapies. When combined with dietary modifications, probiotics promote the growth of beneficial gut microbes, potentially leading to greater symptom relief and improved gut function.
CHALLENGES AND THE PATH AHEAD
Despite the promising potential of microbiome-based therapies, several challenges remain:
1. Regulatory and Standardization Barriers
Ensuring the safety, quality, and consistency of Fecal Microbiota Transplantation (FMT) and other microbiome therapies is essential. This requires the development of rigorous standards and protocols, which must meet regulatory requirements to guarantee the treatments’ effectiveness and safety.
2. Long-Term Efficacy Studies
While initial results are promising, more research is needed to understand the long-term sustainability of microbiome-based treatments. Studies must assess their lasting effects on patients, over an extended period of time.
3. Patient and Physician Education
The widespread adoption of microbiome therapies depends on raising awareness among both patients and healthcare providers. Education will be essential to ensure that these innovative treatments are properly understood and integrated into clinical practice.
A NEW ERA IN IBD MANAGEMENT IS HERE!

The future of IBD care is looking brighter than ever! Thanks to the exciting possibilities microbiome-based therapies are offering. These therapies are not just about addressing symptoms. They target the root causes of gut imbalances, potentially transforming how we treat conditions like Crohn’s Disease and Ulcerative Colitis. By restoring balance to the microbiome, these therapies could provide lasting relief for patients, improving their long-term health and overall quality of life.
As we continue to explore the microbiome’s incredible potential, IBD care is entering a remarkable new chapter!
If you are a physician treating patients with gut health issues (on a regular basis), Crohn’s and Colitis Awareness Week is the perfect time to get involved in something transformative. Joining MDForLives allows you to contribute to the research shaping the future of IBD care and impact how patients are treated.
Let us collaborate and create lasting change in the way we manage IBD.
REFERENCES:
- The future of microbiome‐based therapeutics
www.pmc.ncbi.nlm.nih.gov - The practice of fecal microbiota transplantation in inflammatory bowel disease
www.pmc.ncbi.nlm.nih.gov - Crohn’s disease and ulcerative colitis
www.betterhealth.vic.gov.au

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.