When we think about mosquito-borne diseases, it’s almost automatic for names like malaria and dengue to pop into our heads. These two diseases have been the main focus of global health concerns for decades, dominating discussions, media coverage, and public health efforts. But in this hyper-focus on malaria and dengue, we tend to overlook other mosquito-borne diseases that are creeping into our societies – often with little to no warning. One such disease that has not received enough attention is Oropouche Virus Disease (OVD).
If you’ve never heard of Oropouche before, don’t worry; you’re not alone. Despite its presence for over half a century and increasing cases, oropouche virus news hasn’t garnered the same attention as malaria or dengue virus. This lack of awareness can be attributed to its relatively lower prevalence and the absence of a global pandemic. However, this doesn’t diminish its potential threat!
“On May 27, 2024, Cuba’s Ministry of Public Health reported Oropouche virus outbreaks in Santiago de Cuba and Cienfuegos provinces.” – World Health Organization
So, what exactly is OVD, and why should it be on every healthcare professional’s radar? Let’s dive into the details of this virus and understand the importance of paying attention to this emerging threat.
A COMPREHENSIVE OVERVIEW OF OROPOUCHE VIRUS DISEASE
Oropouche Virus Disease is an arboviral infection caused by the Oropouche virus (OROV), a segmented single-stranded RNA virus. This virus belongs to the genus Orthobunyavirus within the Peribunyaviridae family. It primarily circulates in Central and South America and the Caribbean, making it a significant concern for those regions. However, with climate changes and increased human activities, its potential spread to new areas warrants attention.
The Oropouche virus is transmitted to humans mainly through the bite of the Culicoides paraensis midge, which thrives in forested areas and near water bodies. Certain Culex quinquefasciatus mosquitoes are also implicated in transmission. The virus is thought to exist in both epidemic and sylvatic cycles.
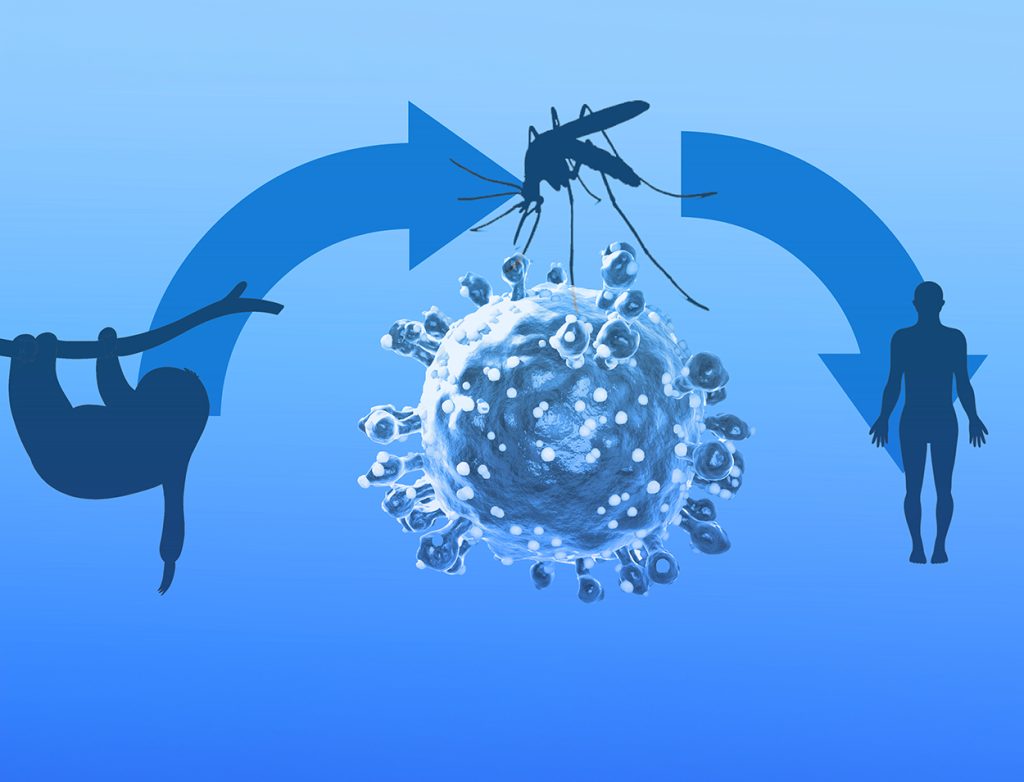
In the sylvatic cycle, vertebrate hosts include sloths, primates, and potentially birds. However, a specific arthropod vector for this cycle has not yet been definitively identified. On the other hand, in the epidemic cycle, humans act as the amplifying host, and the primary vector remains the Culicoides paraensis midge.
Notably, no evidence suggests that the Oropouche Virus Disease can be transmitted directly from person to person.
OROPOUCHE VIRUS SYMPTOMS AND DISEASE PROGRESSION
Symptoms of Oropouche Virus Disease typically resemble those of dengue, making diagnosis challenging. They usually begin to appear between four to eight days after the initial bite from an infected midge. The onset is often abrupt, characterized by fever, chills, headache, joint pain and stiffness, and occasional nausea and vomiting.
The oropouche virus symptoms usually persist for up to five to seven days. While severe cases are rare, oropouche fever symptoms can sometimes lead to complications such as aseptic meningitis. Most individuals recover within a week, though some may experience a prolonged recovery period lasting several weeks.
Currently, no specific antiviral treatments or vaccines are available for OVD. Management relies on symptomatic oropouche fever treatment and supportive care.
MANAGING OROPOUCHE VIRUS DISEASE: ESSENTIAL STEPS FOR HEALTHCARE PROFESSIONALS
Here’s what healthcare professionals should do for effective oropouche fever treatment:
- Enhance Diagnostic Skills: Incorporate Oropouche Virus Disease into your differential diagnosis toolkit, especially in patients with fever, joint pain, and a travel history to endemic areas. Utilize advanced diagnostic tests and consult with specialists if needed to confirm cases.
- Integrate Surveillance Systems: Advocate for and participate in enhanced surveillance systems to track and report cases of oropouche virus transmission. This helps identify trends, outbreaks, and potential hotspots.
- Educate and Empower Patients: Provide clear guidance on recognizing early oropouche virus symptoms and seeking timely medical care. Educate them about preventive measures and the significance of mosquito bite avoidance.
- Advocate for Vector Control: Support and promote community-based vector control initiatives. For instance, request your community to eliminate standing water and use insecticides.
- Collaborate on Research Initiatives: Collaborate with research institutions and public health organizations to understand the oropouche virus transmission cycles, identify vectors, and develop potential vaccines or treatments.
- Implement Proactive Measures: Stay informed about the latest guidelines and protocols for managing mosquito-borne diseases. Implement best practices in patient care, including symptom management and supportive treatment, while remaining adaptable to emerging evidence and recommendations.
- Leverage Technology: Utilize digital health tools and platforms to track patient symptoms, share information with colleagues, and access the latest research on Oropouche Virus Disease. This can enhance diagnostic accuracy and patient management.
- Promote Cross-Disciplinary Collaboration: Work with entomologists, epidemiologists, and other specialists to gain a comprehensive understanding of the virus’s ecology and transmission. This multidisciplinary approach can improve overall disease management and prevention strategies.
- Prepare for Public Health Responses: Be ready to contribute to public health response efforts, including managing potential outbreaks, coordinating with health authorities, and providing accurate information.
- Encourage Reporting and Data Collection: Ensure accurate and timely reporting of oropouche virus news to health authorities. Encourage comprehensive data collection to aid in assessing disease trends and the effectiveness of intervention strategies.
FINAL THOUGHTS
Every healthcare professional’s role in combating emerging diseases like Oropouche Virus Disease (OVD) is crucial and deeply impactful. As the threat of oropouche virus transmission grows, it is vital to broaden the focus beyond well-known diseases to include this rising concern.
Proactive engagement is essential – raising awareness, educating patients, and advancing research efforts can make a significant difference. By incorporating Oropouche Virus Disease into clinical practice and public health strategies, healthcare professionals can help reduce its impact and improve community health outcomes.
Team MDForLives urges all healthcare professionals to stay informed, stay prepared, and lead the charge against this emerging threat.
To truly make a difference in the healthcare sector, register with MDForLives and participate in surveys that enhance patient care, research, and treatment strategies. Your involvement can drive meaningful change and contribute to a healthier future.

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.