Why do we make a fuss about rare mutations in NSCLC? In 2015, they only made up about 1-2% of the entire NSCLC mutation population, though as of 2021, NGS panels have now detected an increase in these incidences.
Perhaps their relevance lies in the models that help oncologists create, enabling us to target the right biomarkers, and utilize innovative precision medicine, to fight against numerous oncogenic driven tumors. The main mutations we will look at are MET, ROS1, and ALK (in part 1), RET, NTRK1 (in part 2), and HER2 (in part 3).

The MET oncogene
MET is a receptor tyrosine kinase, located in chromosome 7 (7q21-q31). It produces HGF (hepatocyte growth factor) receptor, single precursor protein, and extracellular alpha-chain and transmembrane beta-chain, linked by disulfide bonds.
MET is normally activated via ligation with its natural ligand HGF, and in its normal condition, MET activation facilitates cell processes for embryonic development, wound healing, and tissue regeneration.
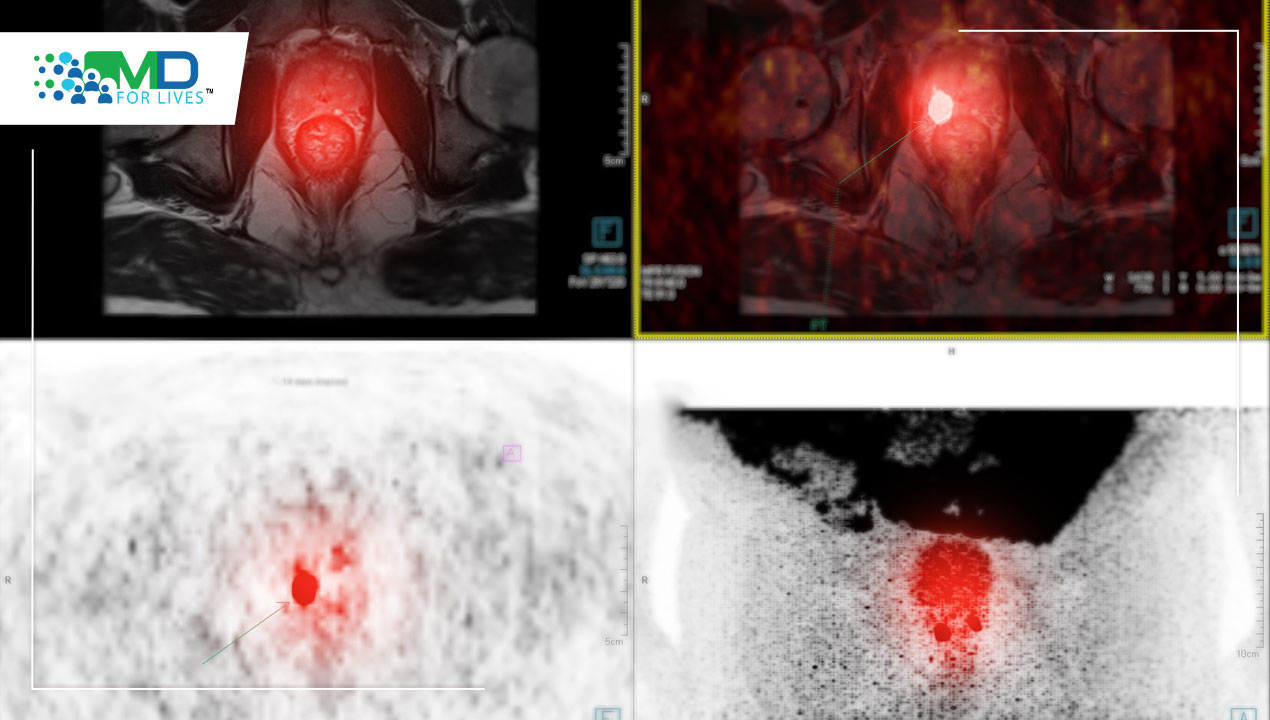
Below you can see MET expression in solid tumors:

As you can see, its prevalence in other cancers is variable, but the highest incidence is seen in lung, ovarian, and breast tumors.
The deregulation of MET in lung cancer is particularly important and can be detected by IHC (immunohistochemistry), copy gain number, the amplification of MET oncogene copy gain number, and the mutation on exon 14.

The MET exon 14 mutation incidences can be seen in the table below. It is much more prominent in lung adenocarcinomas and lung neoplasms than in other diseases.

There have been several studies analyzing cabozantinib (a small molecule inhibitor of the tyrosine kinases c-Met and VEGFR2, which also inhibits AXL and RET) and crizotinib (an ALK and ROS1 inhibitor) in MET-mutated tumors. Below, you can see the responses, confirming positive reactions.

However, there is a multitude of agents (ligand antagonists, receptor inhibitors, and receptor TKIs) that are yet to demonstrate significant Overall Survival (OS) benefit in NSCLC.

Crizotinib – tumor shrinkage was seen in NSCLC patients with intermediate and high MET amplification.

MET amplification on cell lines has been shown to be necessary to obtain control of cell growth, and this high sensitivity has been seen with crizotinib.

The high levels of MET amplification also drive resistance to EGFR-TKIs, as you can see in the FISH assessments below with gefitinib.

In Italy’s METROS trial (2014-2017), crizotinib was tested in MET-amplified or ROS1-translocated NSCLC.

In France, crizotinib was also tested in the AcSé Trial, where MET amplification was clearly tied to the response rate.

Met remains a relevant target, driving tumor growth in approximately 3% of NSCLC with gene amplification (ratio >2.2). Still, prospective studies need to define the best cut-off (ratio 2.2 vs 5). MET amplification is detectable in smokers irrespective of histology. IHC or MET gene copy numbers are not optimal for detecting patients potentially sensitive to anti-MET studies, and new studies with anti-MET agents should be conducted only in carefully selected patients.
ROS1 oncogene The c-ros oncogene 1 (ROS1) is an orphan receptor tyrosine kinase proto-oncogene. In several studies from 2012 to 2015, although ROS1 was not detected in normal heart, lung, ovary, pancreas, and testis tissues, there were low-level expressions in parathyroid glands, eye, larynx, adrenal gland, and skeletal muscle tissues and strong expressions in the cerebellum, peripheric nerves, stomach, small intestine, colon, and kidney. Over the last 5 years, there is definite evidence that ROS1 has clear expressions in multiple tumor types, including NSCLC, oral squamous cell carcinoma, gastric carcinoma, and glioblastoma.

It is calculated that about 10,000-15,000 patients each year develop lung tumors driven by ROS1.

In NSCLC, studies have shown ROS1 to be present in approximately 1% of cases. Generally, those patients are younger, non-smokers, who have developed adenocarcinomas. There is no overlap with oncogenic drivers. Dual ALK and ROS1 inhibition through crizotinib is thought to occur because these receptors bear a 77% identity in their ATP-binding site. In a 2014 study by Shaw, in the New England Journal of Medicine, crizotinib was shown to have a 72% overall response rate in ROS1 rearranged NSCLC, with a 17.6 month duration of response and progression-free survival of 19.2months.

ALK oncogene
Anaplastic lymphoma kinase also known as ALK tyrosine kinase receptor or CD246 is an enzyme that in humans is encoded by the ALK gene. A wide variety of ALK fusions, in which the kinase domain of ALK and the amino-terminal portion of various protein partners are fused, occur in cancer, with echinoderm microtubule-associated protein-like 4 (EML4)-ALK being the most prevalent in non-small-cell lung cancer (NSCLC).
ALK-positive lung cancer occurs in approximately 5% of all lung cancer patients. However, it occurs in approximately 30% of lung cancer patients diagnosed under age 40. About half of ALK-positive lung cancer patients are diagnosed before the age of 50 (compared to about age 70 for lung cancer overall), with many in their 30’s and 40’s, but some even in their teens and twenties.
A kinase selectivity comparison chart, comparing crizotinib, with alectinib (an oral drug that blocks the activity of anaplastic lymphoma kinase) and ceritinib (a drug that targets and binds to the tyrosine kinase receptors and inhibits ALK), demonstrates the effectiveness of crizotinib and ceritinib in ALK (and ROS1)-mutated NSCLC patients.

Indeed, the results from the 2017 ASCEND-14 trial, where mPFS=16.6 months for ceritinib (n=189) versus 8.1 months in the chemotherapy-treated patients (n=187), confirm the effectiveness of ceritinib for ALK-positive NSCLC patients who have metastasis in the brain.
Lorlatinib is a potent and selective next-generation ROS1/ALK inhibitor, capable of blocking crizotinib-resistant ROS1 mutations. In the diagram below, you can see in A, the dose response curves of Lorlatinib (PF-06463922) on ROS1 kinase activity and cell viability in BaF3 cells expressing CD74-ROS1 or ROS1G2032R and ROS1L2026M.
B shows IC50 values on cellular ROS1 activity and cell viability in BaF3 cells expressing CD74-ROS1 and CD74-ROS1 mutants with the indicated inhibitors. Values are shown as mean +/= SD; n >3. C shows inhibition of ROS1 signaling pathways in BaF3 cells expressing the CD74-ROS1G2032R mutant.
In the CROWN trial (2017-predicted end 2024), a phase 3 study comparing lorlatinib with crizotinib as the first-line treatment for advanced ALK-positive NSCLC, patients who received lorlatinib had significantly longer PFS and a higher frequency of intracranial response than those who received crizotinib. The incidence of grade 3 or 4 adverse events was higher with lorlatinib than with crizotinib because of the frequent occurrence of altered lipid levels.
Lorlatinib appears to be a more potent ALK inhibitor than first- and second-generation inhibitors. It is powerful against mutations like ALK G1202R (the most common secondary ALK mutation after disease progression). In untreated patients, lorlatinib could prevent the emergence or even eliminate rare pre-existing subclones harboring ALK resistance. Most importantly, lorlatinib has proven highly effective in treating CNS metastases, with patients who have progressed on second-generation treatments like alectinib and the TKI brigatinib.
Crizotinib has shown poor brain penetrance, so the 87% intracranial response of lorlatinib shows that it may be one of the strongest drugs in preventing brain metastases, and the increased PFS may be due in part to the prevention of CNS metastases. Overall, patients who received lorlatinib reported a significantly greater improvement in global quality of life than those who received crizotinib.