Human epidermal growth factor receptor 2 (HER2) is a member of the ERBB receptor tyrosine kinase family. It is activated by homo- or heterodimerization. As opposed to breast cancer (where HER2 amplification occurs in about 20% of patients and is a predictive marker for anti-HER2 antibodies and TKIs), in 2015 it was calculated that only about 1-2% of lung adenocarcinomas harbored mutations. However, further studies have HER2 expressions in the range of 6%-30%.
Afatinib
In 2010, a phase III trial (Lux-Lung 5) assessed afatinib vs placebo, but OS was not extended. Lux-Lung 1 Phase IIb/III in 2012 confirmed this lack of efficacy. In the NICHE Phase II trial, in patients with NSCLC and the Exon 20 mutation, 53.8% achieved disease control, mPFS was 15.9 weeks and mOS was 56 weeks, again bringing into doubt the potential of the drug.
Major NSCLC biomarker studies
There have been 2 large movements in biomarker-targeting NSCLC studies. In 2012, the French National Cancer Institute (INCa) analyzed patients with EGFR mutations, EML4-ALK translocation, and EGFR T790M, KRAS, BRAF, HER2, and PI3KCA mutations (BIOMARKERS-France study)
Data on 1007 patients in the Lung Cancer Mutation Consortium (LCMC), who had metastatic or recurrent lung adenocarcinomas, and ECOG 0-2, were tested to find HER2 insertions and EGFR deletions.
The most frequent site of disease involvement in HER2 positive patients was the lungs (12%). In wild-type, there was lung involvement in 48% of patients.
Six major treatments were analyzed in the LCMC study:
1. Dacomitinib (a TKI that inhibits EGFR).
2. Trastuzumab (a recombinant humanized IgG1 monoclonal antibody against HER2).
3. Neratinib (an irreversible pan-HER TKI) + temsirolimus (an mTOR inhibitor).
4. Dacomitinib (a TKI that inhibits EGFR) with crizotinib (an ALK and ROS1 inhibitor).
5. Lapatinib (a dual tyrosine kinase inhibitor that interrupts the HER2/neu and EGFR pathways) with trastuzumab and bevacizumab (a monoclonal antibody that inhibits VEGF – vascular endothelial growth factor).
6. STA-9090/Ganetespib – a heat shock protein 90 (HSP90) inhibitor.
The mOS of the patients that received HER2 therapy was 2.09 years vs 1.37 years without targeted therapy. The survival of HER2 wild-type patients was 2.62 years. Among the patients who were treated with targeted therapy, 50% were alive vs 33% who received systemic therapy alone.
Dacomitinib
Dacomitinib, a second-generation EGFR-TKI, works by inhibiting the signaling from both heterodimers and homodimers of all of the members of the HER family. In the Archer 1050 Phase III study of dacomitinib vs the EGFR TKI gefitinib, dacomitinib had a superior PFS (14.7 vs 9.2 months) and OS (34.1 vs 26.8 months). The incidence of diarrhea, skin rash, mucositis, and dose reductions was higher with dacomitinib, while hepatic toxicity was higher with gefitinib.
Dacomitinib has clearly shown efficacy in patients whose tumors harbor HER2 mutations or amplification. Among 30 patients treated with dacomitinib in a phase II study, 3 patients with exon 20 mutation achieved PR, while no patients with HER2 amplification obtained an objective response. Dacomitinib inhibits EGFR, HER2, and HER4 tyrosine kinases; however, these results suggest that the HER2-mutant population is widely heterogeneous and only a limited group of patients may benefit from this treatment.
Neratinib
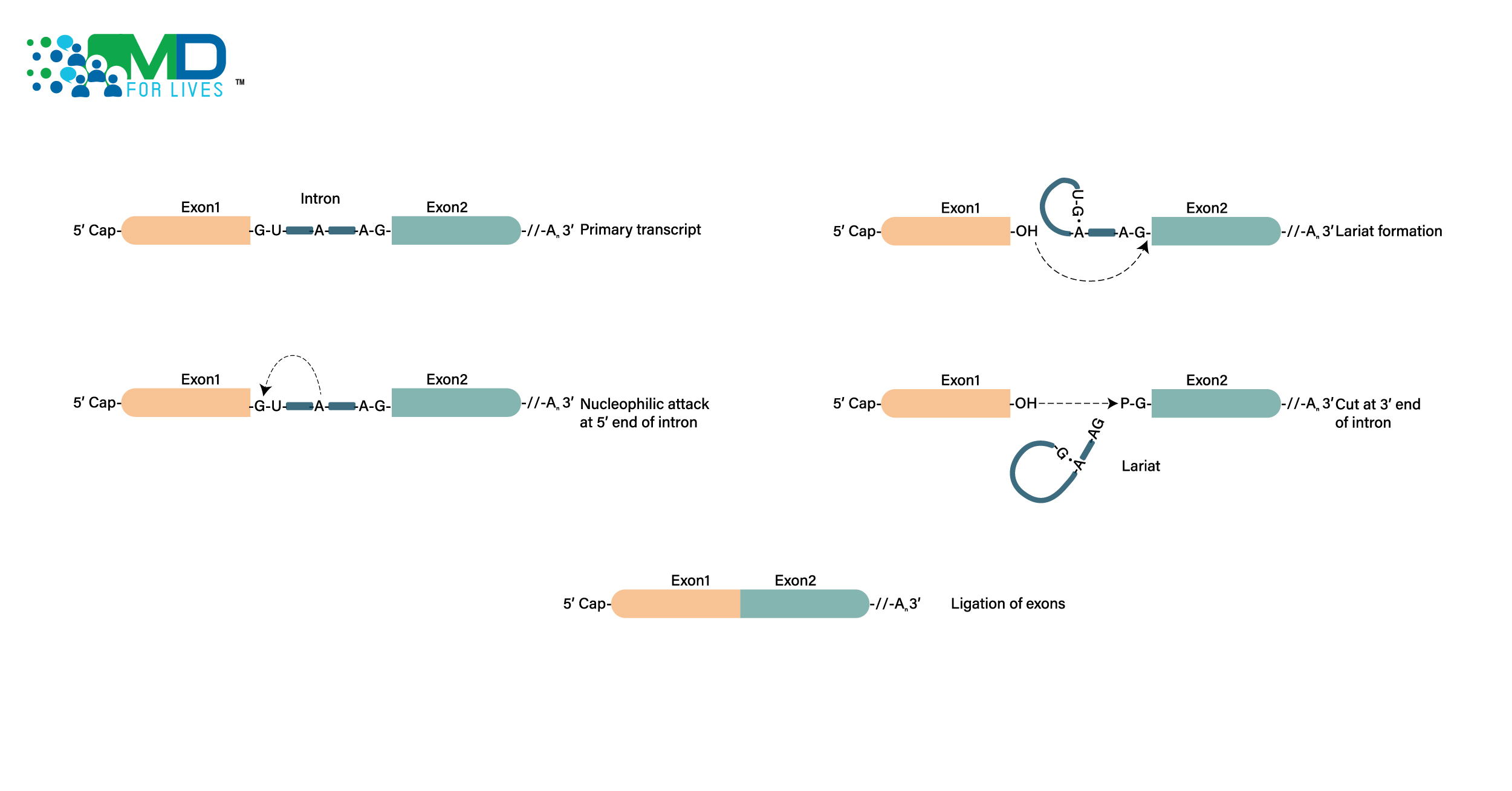
In the phase 2 SUMMIT basket trial, assessing an EGFR-mutant NSCLC cohort of 11 patients with exon 18 mutations, neratinib was pitted against gefitinib, erlotinib, osimertinib, and afatinib. Neratinib had a CBR (clinical benefit ratio) of 80%, with DOR of 7.5 months and PFS of 9.1 months, with no hospitalizations and no grade 3-4 diarrhea. What is most interesting was the strong HER2 responses found in the studies. Further analyses on mouse xenografts in 2019 (see the diagram below) have proven strong tumor growth inhibitory activity, and further trials make neratinib one to watch in the future.
There are several other studies underway, looking at patients with HER2 in NSCLC, and more physicians are now realizing the possibilities of targeting this biomarker.
In the 2016 EUHER2 cohort, patients with advanced NSCLC were assessed, a known HER2 exon-20 insertion, and treated with chemotherapy and/or HER2-targeted drugs.
In 101 patients (median age 61, 62% women, 60% never smokers), where all tumors were adenocarcinomas: 5 EGFR mutations, 1 ALK translocation, and 1 ROS translocation were observed, OS was 24 months, and in first line, ORR was 43.5% with 6 months PFS, while in second line, ORR was 10% and 4.3 months PFS. Sixty-five patients received HER2 targeted therapies (trastuzumab = 14, afatinib = 9, lapatinib = 5, T-DM1 = 1). ORR was 50.9% with trastuzumab or TDM1 (trastuzumab emtansine) with a PFS of 4.8 months.
This confirmed the chemosensitivity of HER2-driven NSCLC, proving the need for more research and physician commitment in this field.
Although dacomitinib, afatinib, and neratinib have produced some effects in patients with HER2-mutant lung cancers, the low response rates of 0% to 19% have stalled further development. Fortunately, into the field have arrived two strong new players, kicking HER2 inhibition back into gear. These are TDXd and TDM1.
Trastuzumab deruxtecan
Trastuzumab deruxtecan (T-DXd) is an antibody drug conjugate (ADC) with three components:
- It is a humanized anti-HER2 IgG1 Mab with the same amino acid sequence as trastuzumab.
- It is a topoisomerase I inhibitor payload, an exatecan derivative.
- It is a tetrapeptide-based cleavable linker.
At ASCO 2020, the interim results of the DESTINY-Lung01 study were posted, assessing trastuzumab deruxtecan in patients with HER2-mutated metastatic NSCLC.
From the data, we can see a 61.9% ORR, with a DCR of 90.5% and 14-month PFS.
The median treatment duration was 7.76 months (range, 0.7-14.3 months). The most common TEAEs associated with dose reduction were fatigue (11.9%) and nausea (9.5%). The most common TEAEs associated with dose interruptions were decreased neutrophil count (19.0%) and lung infection (7.1%). There were 5 patients with TEAEs associated with death; none were related to treatment.
Ado-Trastuzumab emtansine (T-DM1)
T-DM1 is a HER2-targeted ADC linking trastuzumab with the antimicrotubule agent emtansine.
In 18 patients with advanced HER2-mutant lung adenocarcinomas, with an average of two prior systemic therapies, the partial response rate was 44%. Responses were seen in patients with HER2 exon20 insertions and point mutations in the kinase, transmembrane, and extracellular domains. HER2 IHC ranged from 0 to 2+ and did not predict response. Responders also had low HER2 protein expression measured by mass spectrometry. Median PFS was 5 months, with thrombocytopenia and elevated hepatic transaminases the main grade 1 or 2 reactions. There was a zero-discontinuation rate and no deaths.
Below is the swimmer plot of PFS:
The AEs are shown below:
The HER2 biomarker analysis table can be seen below, with all 18 patients having HER2-activating mutations (identified by NGS). Two patients had concurrent HER2 amplification, and both these patients achieved stable disease and partial response. There was no association between IHC and response to T-DM1. Three of six patients with partial responses showed increased HER3 expression, while five of six tested by mass spectrometry showed low levels of HER2 protein.
In NSCLC, chemotherapy with pemetrexed remains the current standard of care for patients with the HER2 mutant. The benefit of immune checkpoint inhibitors in patients with HER2 aberrations is still unknown; response rates may be low like in other oncogene-driven cancers (EGFR, ALK, and MET exon 14 mutants). Indeed, none of the seven patients in this study who received prior anti-pd-1 inhibitors achieved a response. Further studies are needed to choose the best combinations or monotherapies in targeted and non-HER2-targeted therapies.
If, however, these results are repeated in both TDM-1 and TDXd, a new standard of treatment will soon be on the horizon in NSCLC patients. HER2 is here to stay and is one of the more emerging dark horses in NSCLC genetics. If the trend continues, physicians might well be best ordering HER2 among their list of biomarkers, alongside the EGFR and PD-L1 expressions.