Errors in medical surveys are like weak links in a chain. No matter how robust and resilient the rest of the chain is, a couple of weak links are enough to break it. Suppose a set of responses inaccurately inflates or deflates a certain metric (like the prevalence of a symptom or the effectiveness of a treatment). It could mislead researchers into making incorrect generalizations about the population being studied. Especially in small sample sizes, one inaccurate response can adversely influence the mean, median, and other statistical measures. This can lead to skewed averages, incorrect correlations, and faulty conclusions.
It is crucial to maintain the authenticity and reliability of survey responses. Survey data plays a vital role in medical research, healthcare policy-making, and clinical decision-making. It informs treatment protocols, shapes healthcare guidelines, and influences public health strategies, all of which directly impact patient care. A stringent pre-screening process helps ensure the accuracy of the data by verifying the eligibility and credibility of respondents. It filters out ineligible participants and retains the integrity of research findings.
HOW PRE-SCREENING PROCESS IMPROVES RELIABILITY AND VALIDITY OF SURVEYS
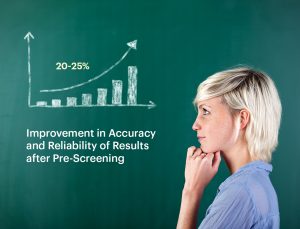
Pre-screening is not just a preliminary step. It is the cornerstone of accuracy in medical research. Meticulously identifying suitable participants allows researchers to enhance the reliability and validity of their survey data, leading to more robust and actionable outcomes.
To achieve this, researchers carefully consider factors such as age, gender, specific health conditions, and other demographic variables. These criteria help ensure that the study group is homogeneous enough to minimize confounding variables while still being representative of the larger population. This careful selection process is essential for producing data that can lead to meaningful and applicable conclusions. It ultimately improves patient care and health outcomes.
Data Accuracy: Pre-screening enhances data accuracy by ensuring participants meet the study’s criteria. For instance, a study on diabetes management in older adults cannot be conducted without a rigorous pre-screening process. Participants who are too young or do not have diabetes might be included, skewing the results. A well-organized pre-screening process reduces the rate of survey rejections by eliminating the risk of outliers.
Reducing Errors: Pre-screening minimizes the likelihood of errors and inconsistencies in the data by weeding out ineligible participants from the start. This step is crucial in large-scale studies, where minor errors can have significant repercussions.
Improving Validity: Pre-screening contributes to internal validity (the extent to which the study measures what it intends to) and external validity (the extent to which the findings can be generalized). The results are more likely to reflect authentic relationships and trends with the right participants.
WHAT ARE SOME OF THE PERSISTENT CHALLENGES IN PRE-SCREENING?
While pre-screening is crucial for enhancing the reliability and validity of surveys in medical research, it is not without its challenges. Researchers must navigate several obstacles to ensure the pre-screening process is effective and efficient. Below are some of the challenges associated with pre-screening:
Resource Intensive: Pre-screening can be resource-intensive, requiring significant time, money, and personnel. Developing thorough criteria and conducting detailed assessments can stretch resources, particularly in large-scale studies.
Complex Criteria: Developing and applying complex pre-screening criteria can be challenging. As research becomes more specialized, the criteria for participant selection may become more intricate, necessitating a more nuanced approach to pre-screening.
Participant Attrition: While pre-screening is designed to select the best candidates, it can also lead to higher dropout rates. Some participants may decide to refrain from continuing if they find the pre-screening process too rigorous or invasive.
IMPLEMENTING BEST PRACTICES FOR EFFECTIVE PRE-SCREENING PROCESS
Addressing pre-screening challenges requires careful consideration of best practices to ensure the process is efficient and effective. Implementing these best practices helps researchers mitigate the difficulties and enhance the overall quality of their studies. Below are some critical strategies for optimizing the pre-screening process:
Clear Criteria: To avoid ambiguity, pre-screening criteria must be clear, specific, and well-justified. This clarity helps ensure that the right participants are selected and the process is transparent, enhancing the reliability and validity of surveys.
Regular Updates: Pre-screening protocols should not be static. Regular updates based on new research findings, feedback from previous studies, and evolving best practices are essential for maintaining their relevance and effectiveness.
Training and Quality Control: Training research staff in pre-screening procedures and implementing robust quality control measures are critical for ensuring the reliability of a survey. These steps help maintain consistency, reduce errors, and ensure the pre-screening process is executed correctly.
FUTURE DIRECTIONS IN PRE-SCREENING FOR MEDICAL RESEARCH
A wide array of cutting-edge innovations are reshaping the future of pre-screening in medical research. While advances in artificial intelligence (AI) and machine learning are enhancing the speed and accuracy of participant selection, standardized protocols in multi-center studies are bringing consistency and precision across various research settings.
Staying on top of these advancements will help researchers improve data quality and achieve more reliable and impactful results from medical surveys, ultimately enhancing patient care and health outcomes.
As the norms of medical research are continuously redefined by technological advancements, healthcare professionals and researchers must prioritize pre-screening in their studies to uphold the reliability of a survey, and eventually contribute to more accurate research outcomes and better patient care.
If you are a healthcare professional ready to contribute to medical research, Join MDForLives and make your voice heard!
Your participation in our paid physician surveys can help shape better healthcare initiatives and improve patient care.
Do you have a story to share about new medical breakthroughs or research? Write to us at collaboration@mdforlives.com.
REFERENCES:
- Best Practices in Pre-Screening Includes Use of Technology
www.advarra.com - Clinical Trials – The Screening Process
genesisresearchservices.com
A. Royden D’Souza is a professional writer with over 5 years of experience in the healthcare industry. He holds an engineering degree and has worked with several brands to meet their content requirements. He is passionate about writing engaging content for healthcare professionals, allied healthcare professionals, and nurses.






