Cervical cancer, a formidable health concern impacting women globally, has spurred a collective effort to refine preventive measures. As we mark Cervical Cancer Awareness Month, it’s crucial to highlight the significant strides in raising awareness and promoting proactive health practices. In the previous year (2023), approximately 13,960 new cases of invasive cervical cancer were identified in the United States. Moreover, the American Cancer Society estimated that 4,310 women would succumb to cervical cancer during the same period. These figures highlight the ongoing need for awareness, early detection and continuous improvement to prevent cervical cancer.
Over the years, conventional screening techniques, notably Pap smears, have been instrumental in early detection, acting as a frontline defense to prevent cervical cancer. However, the dynamic arena of preventive measures for cervical cancer is undergoing a transformative shift. This blog embarks on an exploration of the imperative to transcend the reliance on Pap smears, delving into the necessity of adopting a comprehensive approach to prevent cervical cancer effectively.
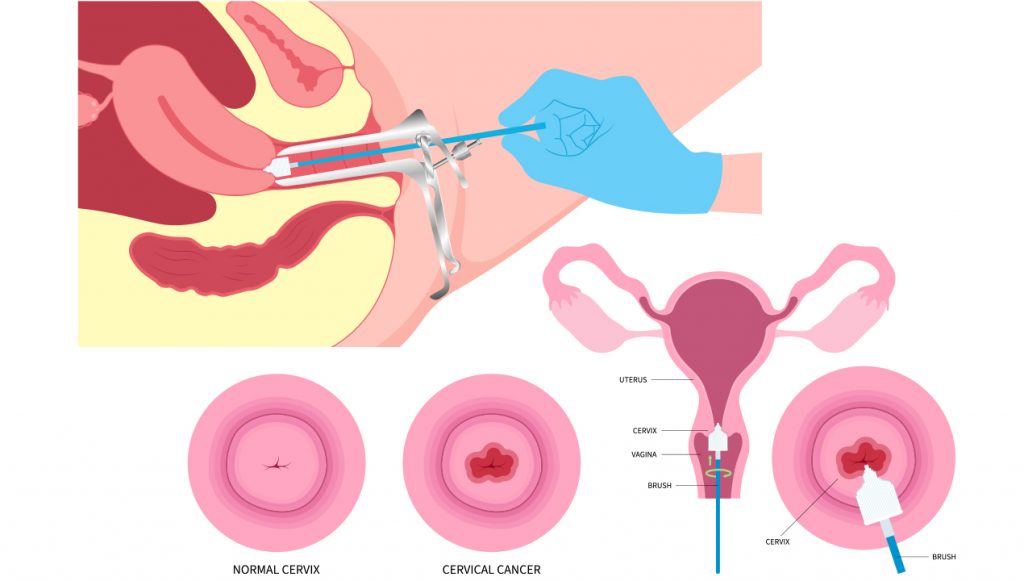
PAP SMEARS: UNDERSTANDING ITS LIMITATIONS
While Pap smears have undoubtedly played a crucial role in the early identification of abnormal cervical cells, it is essential to acknowledge their inherent limitations. These screening methods operate primarily by detecting changes in cell morphology, offering valuable insights into potential precancerous or cancerous developments. However, this singular focus on cell morphology poses a limitation as it may overlook other critical factors contributing to the onset and progression of cervical cancer.
One notable blind spot in Pap smear analysis is its inability to consistently identify persistent infections caused by high-risk human papillomavirus (HPV) strains. HPV infections, particularly those of the high-risk variety, are a primary precursor to cervical cancer. Pap smears may not capture the subtleties of persistent HPV infections, potentially leading to false assurances when the underlying risk persists.
Moreover, the periodic nature of Pap smears introduces a temporal dimension that, while effective in many cases, also presents challenges. The recommended intervals between screenings may inadvertently create windows of vulnerability, allowing potential risks to escalate unchecked. In some instances, the delayed detection of evolving abnormalities may result in a missed opportunity for early intervention, compromising the effectiveness of preventive measures.
Recognizing these limitations highlights the critical need to supplement traditional Pap smears with more comprehensive approaches that can prevent cervical cancer. Embracing evolving methodologies that go beyond mere morphological assessment becomes imperative to enhance the precision and timeliness of cervical cancer detection, ultimately contributing to more effective preventive strategies.
EMBRACE THE COMPREHENSIVE PARADIGM
The question that must arise in the reader’s mind is – “If not Pap smears, then what’s the way forward?” The answer lies in embracing a revolutionary paradigm that transcends the limitations of traditional screening methods. Instead, envision a multifaceted strategy where HPV vaccination takes center stage, acting as a formidable shield against the very origins of cervical cancer.
This proactive approach goes beyond the routine Pap smears, incorporating cutting-edge technologies such as regular HPV testing. By synergizing these two methods, physicians can create a more comprehensive and nuanced analysis of risk factors, providing a heightened level of precision in the detection and preventive measures for cervical cancer.
THE POWER OF HPV TESTING & VACCINATION IN CERVICAL CANCER PREVENTION
Human Papillomavirus (HPV) stands as a pervasive and formidable foe in women’s health, particularly when it comes to cervical cancer. In the pursuit of more effective prevention, HPV testing and vaccination emerge as powerful tools, reshaping the landscape of cervical cancer prevention.
HPV Testing

Unlike traditional Pap smears, which primarily identify abnormal cell changes, HPV testing allows for the direct determination of the virus responsible for these changes. This method provides a more precise and early detection of high-risk HPV strains, offering a proactive approach to prevent cervical cancer.
In routine HPV testing, a sample of cervical cells is collected and the presence of HPV DNA is analyzed. This not only helps in identifying women at higher risk but also enables healthcare providers to tailor surveillance and intervention strategies to prevent cervical cancer accordingly. Integrating HPV testing into routine screenings enhances the sensitivity and specificity of cervical cancer detection, making it an indispensable component of modern preventive healthcare.
HPV Vaccination

HPV vaccination serves as a pivotal cornerstone in the fight against cervical cancer. By immunizing individuals against the most common high-risk HPV strains, vaccines effectively reduce the risk of HPV infection and subsequent development of cervical lesions. Typically administered in adolescence, HPV vaccination has demonstrated remarkable success in preventing cervical cancer and other HPV-related cancers.
The vaccines primarily target HPV types 16 and 18, which are responsible for a significant portion of cervical cancer cases. Vaccines act as powerful shields by inducing a robust immune response against these strains, fortifying the body’s defenses against potential infections. Moreover, as part of a broader strategy, vaccines contribute to the reduction of overall HPV prevalence in the population, creating a cascading effect in decreasing cervical cancer incidence.
The Synergy of HPV Testing and Vaccination
Combining HPV testing with vaccination forms a comprehensive and forward-looking approach to prevent cervical cancer. Routine HPV testing allows for the early identification of persistent infections, guiding healthcare providers in tailoring interventions for high-risk individuals. Simultaneously, vaccination addresses the root cause by preventing HPV infection in the first place.
This synergistic strategy not only provides a more nuanced analysis of cervical cancer risk factors but also empowers individuals with preventive measures for cervical cancer. The integration of HPV testing and vaccination into women’s health initiatives represents a paradigm shift, emphasizing precision, prevention and a proactive stance against cervical cancer.
EMPOWERING WOMEN: YOUR PRIMARY DUTY AS AN ONCOLOGIST IN THE FIGHT AGAINST CERVICAL CANCER

While innovative technologies and medical breakthroughs play a crucial role in advancing the fight against cervical cancer, the foundation lies in empowering women to take charge of their health. As an oncologist, you have a unique opportunity to make a profound difference in this battle.
Here are some ways you can contribute:
- Be a Knowledge Champion
- Become a trusted source of information: Combat misinformation and empower women with accurate, clear and accessible information about cervical cancer, HPV and medication for cervical cancer patients.
- Embrace clear communication: Use simple language, avoid medical jargon and actively listen to their questions and concerns.
- Normalize open dialogues: Create an environment where women feel comfortable discussing their sexual health and concerns without judgment.
- Advocate for Prevention
- Promote the importance of routine screenings: Explain the limitations of Pap smears and the benefits of HPV testing and other screening methods.
- Highlight the power of vaccination: Encourage HPV vaccination as a crucial preventative measure for both men and women.
- Address access barriers: Help women navigate insurance coverage, language barriers and logistical challenges to ensure they receive screenings and follow-up care.
- Foster Patient-Centered Care
- Tailor your approach to individual needs: Consider cultural beliefs, socioeconomic factors and personal preferences when offering recommendations and support related to lifestyle changes for cervical cancer.
- Embrace shared decision-making: Involve women in their treatment plans, clearly explaining options and potential outcomes.
- Connect them to resources: Provide information about support groups, mental health services and other social determinants of health that can impact their well-being.
Remember, your role extends beyond providing medical expertise. By prioritizing clear communication, advocating for preventive measures for cervical cancer and fostering patient-centered care, you can become a powerful advocate for women’s health and empowerment in the fight against cervical cancer.
Additional tips:
- Utilize educational materials: Distribute pamphlets, infographics or videos in diverse languages with concise and accurate information.
- Partner with community organizations: Collaborate with local groups and healthcare providers to reach underserved communities and spread awareness.
- Engage in advocacy efforts: Raise awareness about how to prevent cervical cancer through public talks, workshops or social media campaigns.
By combining medical expertise, compassion and a commitment to patient education for cervical cancer, you can make a significant contribution to a future where cervical cancer becomes a preventable disease.
CONCLUSION

Moving beyond Pap smears is a step towards a more holistic and practical approach to prevent cervical cancer. By embracing comprehensive strategies that include vaccination, regular HPV testing, patient education for cervical cancer, lifestyle modifications, improved healthcare access and collaborative research efforts, we can make significant strides in reducing the incidence and impact of this preventable disease. As we continue to evolve our understanding of cervical cancer, a multifaceted approach ensures that we address the complexities of this health challenge and empower women to prioritize their well-being.
With MDForLives, you can now share your unique perspective through paid medical surveys and insightful articles, while gaining access to exclusive webinars and enriching discussions.
References:
- HPV Vaccination and Testing
www.ncbi.nlm.nih.gov - What are the benefits and limitations of screening for cervical cancer?
www.cancer.ca - Cervical Cancer
www.webmd.com - Cervical Cancer Screening
www.cancer.gov

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.