Over 13 million people will have a stroke each year and around 5.5 million people will die as a result. According to world-stroke.org, stroke has already reached epidemic proportions. Globally 1 in 4 adults over the age of 25 will have a stroke in their lifetime. 13.7 million people worldwide will have their first stroke this year and five and a half million will die as a result. Current trends suggest that the number of annual deaths will climb to 6.7 million annually without appropriate action. Ischemic stroke stands out as one of the most critical neurological emergencies today, and the MDforLives explores both the causes and the treatment approaches for ischemic stroke.
Types of Strokes
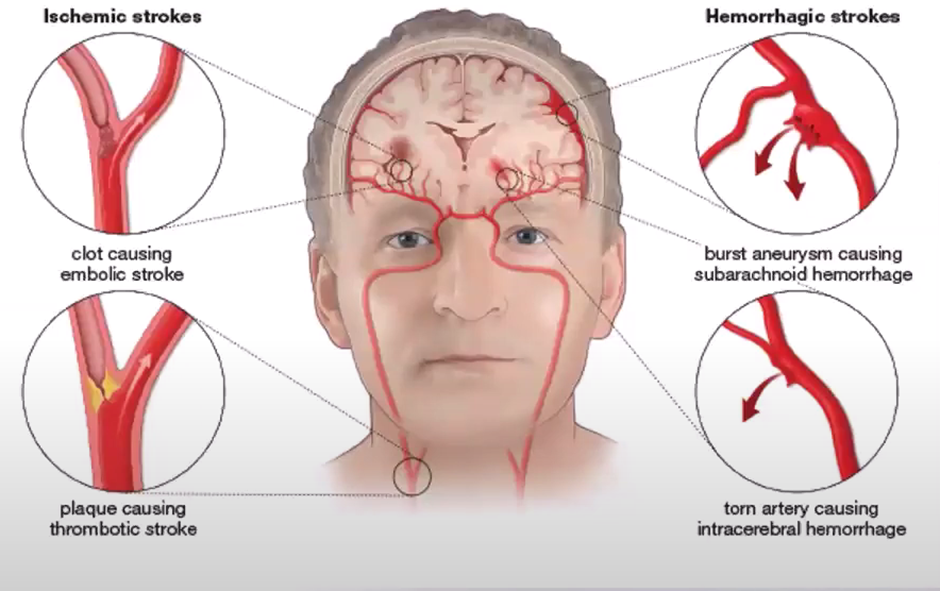
There are 2 types of strokes:
- Ischemic – comprising of Ischemic stroke and Transient ischemic attack (TIA)
- Hemorrhagic – for example, non-traumatic intracerebral/intraventricular hemorrhages, aneurysms, arteriovenous malformation (AVM), intracranial venous thrombosis, and other vascular issues,
Pathogenesis of Cerebrovascular Disease
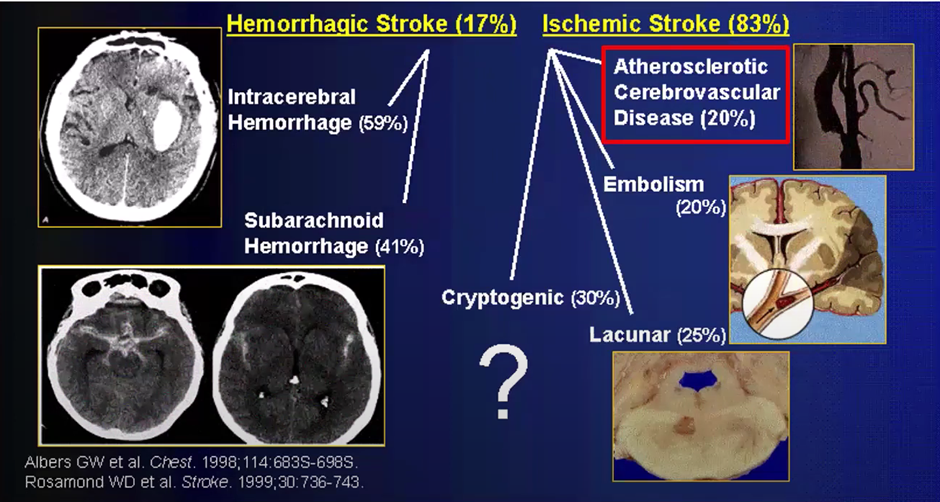
Ischemic stroke accounts for nearly 85% of all strokes, of these:
- 20% are caused by atherosclerotic cerebrovascular disease. This is plaque build-up in the artery.
- 20% of ischemic stroke is caused by embolism, most usually from the heart as a cardiac embolism, due to atrial fibrillation.
- 25% of strokes are lacunar strokes. These are small vessel strokes usually caused by high blood pressure/uncontrolled high blood pressure.
- 30% of strokes are cryptogenic. These are now called embolic strokes of undetermined source (ESUS). It is unknown what caused the stroke in these patients, though it is believed to be from an embolic source (Embolism occurs when a piece of a blood clot, foreign object, or other bodily substance becomes stuck in a blood vessel and largely obstructs the flow of blood).
What Causes Ischemic Stroke?
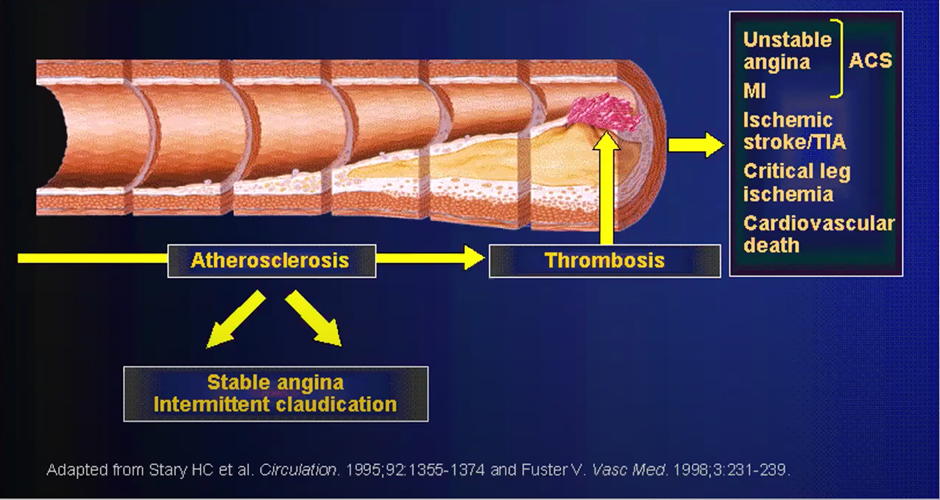
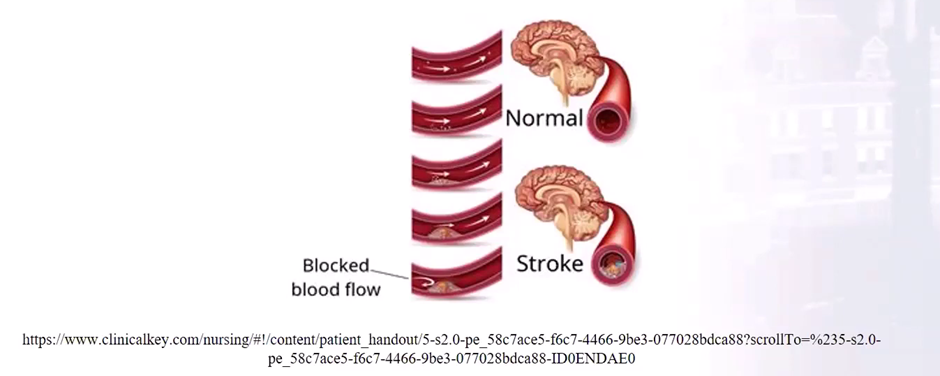
Ischemic strokes are the obstruction of blood flow to the brain that leads to ischemia (lack of oxygen) and infarct (tissue death). This involves both ischemic stroke and transient ischemic attack (TIA).
You can see in the image below the blocked flow, very much like a blocked pipe, but in this case blood and oxygen do not make it to the brain.)
Symptoms of Ischemic strokes
TIA are known as ‘mini-strokes’ (this is where patients suffer all the symptoms of a stroke, but they continue with their day, or sleep on the issue., hoping the symptoms will resolve). TIA are a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction. Of patients presenting with an ischemic stroke, 7-40% had a TIA before their stroke. A patient that has one or more TIA’s are 10 times likely to have a stroke, and a third go on to have a severe stroke within a year (Easton J.D, Saver J.L, Albers GW, et al. Stroke 2009;40;2276-2293).
About 41% of TIA’s last less than an hour. Interestingly, if you look at MRI scans in patients with TIA symptoms lasting less than 1 hour, 30% of patients will show positive for having a stroke using diffusion weighted imaging (DWI), and 50% if the symptoms lasted up to 12 hours.
Stroke will occur within 90 days in 10-20% of TIA patients, and approximately 50% will occur within 24-48 hours. (Thomas J DeGraba, Clinical Stroke & Traumatic Brain Injury Research Program, Naval Medical Center, May 2007).
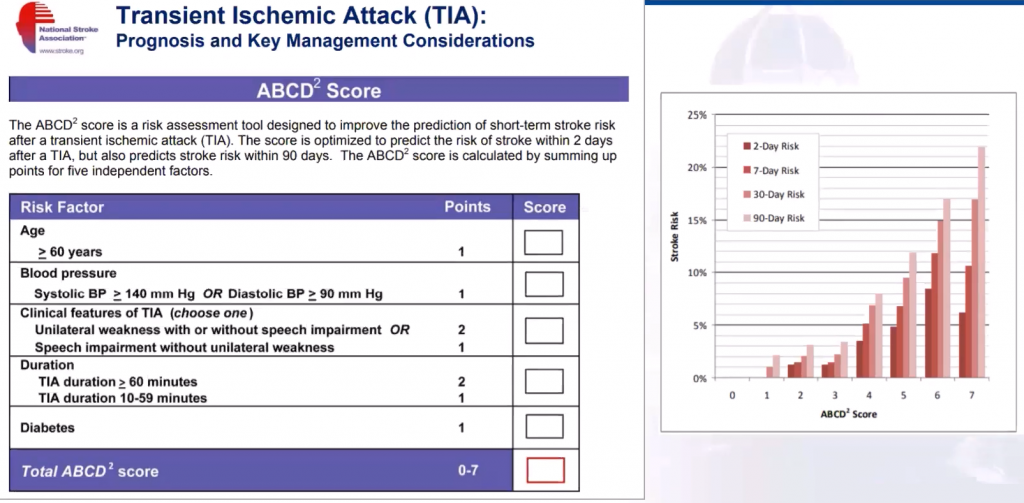
When patients arrive at the emergency department with a probable TIA, a scale that is being used (created by the National Stroke Association) to assess severity is the ABCD2 score. This will look at age, blood pressure, clinical features, TIA duration and any history of diabetes, to determine what the probability is that a patient will go on to have a stroke. You can see a breakdown below. In the chart to the right, you can see, the higher your score the higher the risk of stroke. The stroke scale helps HCPs determine whether a patient can remain on outpatient or needs to be admitted into hospital immediately.
Risk Factors for Ischemic Stroke
The risk factors for ischemic stroke include those within a patient’s control, and those outside:
Within control:
- Hypertension
- Smoking
- Diabetes
- Diet
- Physical activity
- Obesity
- High cholesterol (carotid artery disease)
- Atrial fibrillation
- Other heart disease
- Sickle cell anemia
Outside control:
- Age (your chance of having stroke doubles for every decade of life after 55)
- Family history (first degree relative has a stroke or heart attack before 65)
- Race (In the USA, according to the National Institute of Child Health and Human Development, Hispanic Americans and American Indian/Alaska Natives are at greater risk than whites are for having a stroke but are at less risk than African Americans.
- Gender (women have more strokes than men – the use of birth control pills, pregnancy, history of preeclampsia, or gestational diabetes, along with smoking, post-menopausal hormone therapy, all pose an especial stroke risk for women)
- Prior stroke, TIA or heart attack.
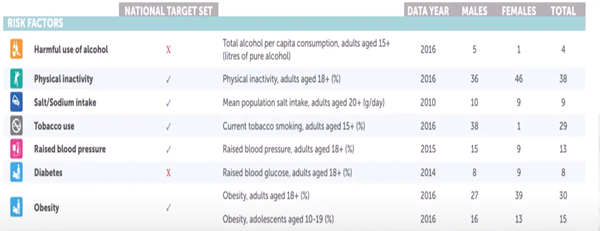
Study on Ischemic strokes
A study by the Sheikh Khalifa Stroke Institute (SKSI) in 2020 showed the % of the United Arab Emirates population with risk factors for stroke, with physical activity, obesity and tobacco use being an important cause of stroke:
Ischemia penumbra:
When a patient has had a stroke, there is an area known as the Ischemic penumbra. The area where the stroke is, where the dead issue can be found, is the core of the infarction. Ischemic penumbra is around the core infarct with minimally surviving cells. This is the target for medical and pharmacological interventions. As you can see below, the target it so to reduce the size of the stroke that has happened in the dead tissue, to stop it expanding into the penumbra. Within an hour of a hypoxic ischemic event, the core of infarction already starts dying, and those minimally surviving cells (the ischemic penumbra) are at greatest risk for neuronal death, but they are alive and salvageable. Because this area has decreased perfusion, frequently permissive hypertension is performed, to keep blood flow to this area. Blood sugar control is key at this stage, to keep the tissue alive.
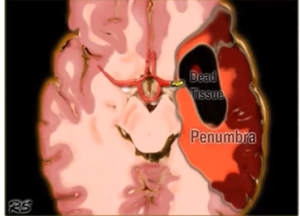
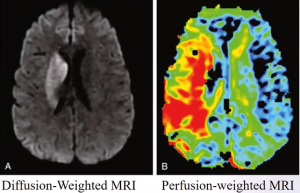
Below you can see a diffusion-weighted and perfusion-weighted MRI of a stroke patient, the area In red is the region most at risk of becoming infarcted, so this must be targeted for salvage therapy
Ischemic Stroke Treatment Options
For Acute Revascularization (opening up of the vessels):
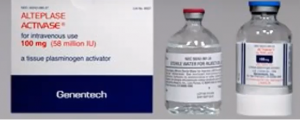
- Intravenous thrombolytic therapy is recommended. This can be done with Alteplase an IV tissue plasminogen activator (tPA), this must be administered 3-4.5 hours following stroke onset
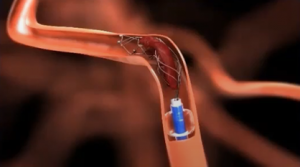
Endovascular Recanalization (mechanical thrombectomy) is an option and must be conducted 6-24 hours since the patient was last known well.
- Combined Intravenous/Intra-arterial (IA)therapy: IA tPA within 3-6 hours of stroke onset, possibly followed by mechanical thrombectomy
- Medical management – if the patient does not come within these specific early timeframes, meaning medical management is the only option/ This includes carotid endarterectomy (removal of plaque blocking carotid artery), angioplasty (going through an artery in the groin, followed by inflating a balloon to expand the narrowed artery, and utilization of a stent to support the opened artery).
Time is brain in ischemic stroke, the longer it takes for the patient to receive therapy, the higher the risk of stroke.
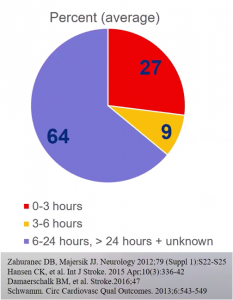
As you can see above, only 36% of patients arriving at hospital with stroke conditions present within the first 6 hours, and only 28% between 6-24hrs, meaning 64% can not get tPA because they are outside the window. This needs to change if we are going to offer the best chance for patients to survive this debilitating illness.
Read also about
Why sporting heroes suddenly collapse with heart attacks
Smart Watches for Atrial Fibrillation Detection

MDForLives is a global healthcare intelligence platform where real-world perspectives are transformed into validated insights. We bring together diverse healthcare experiences to discover, share, and shape the future of healthcare through data-backed understanding.