Glaucoma is one of the most common causes of blindness globally (Quigley and Broman, 2006). Currently, the only modifiable risk factor for glaucoma is intraocular pressure (Lim et al., 2008). The fundamental approach currently is medical therapy, laser treatment and surgical intervention. Historically, surgical intervention has been the last resort to manage glaucoma. This is due to more invasive and more complicated nature of more conventional and established surgical techniques such as filtration surgery and aqueous shunt implants. Given that glaucoma is more prevalent in over 70s, and with the growing number of aging populations, better treatments and less invasive surgical approaches are required.
Considering coexisting other morbidities of the old age, the advent of minimally invasive glaucoma surgery (MIGS) has opened a new chapter in the armamentarium of glaucoma management. There has been an explosion of various techniques and devices in this field. According to the Medicare data{Rathi et al., 2021}, MIGS is superseding all other glaucoma surgeries in the US alone. There are various approaches such as ab interno vs ab externo to implant some these devices. Their target area could be outflow facility or inflow of aqueous humour. Furthermore, they could be conjunctival sparing or minimally invasive bleb forming procedures.
Some of the commonly used trabecular bypass devices are iStent and Hydrus. These devices are gaining popularity amongst glaucoma specialists and cataract surgery for their ease of use during the cataract surgery. They have received CE mark and FDA approval.
Furthermore, techniques such as endoscopic cyclophotocoagulation (ECP) are becoming more attractive in managing glaucoma especially in Europe. This is one of the only MIGS that targets inflow of aqueous humour rather than outflow. MIGS could be performed as a combined procedure during cataract surgery or standalone. Although, there has been much literature endorsing the safety and effectiveness of these devices, there is little discussion about their cost benefit and quality of life. Nonetheless, clinical trials set up strict eligibility criteria, which is less likely to reflect real-world clinical practice. This means the interpretation of the data and generalisability of the information may become more challenging. HORIZON {Ahmed IIK et al., 2021} and COMPARE {Ahmed IIK et al., 2020} trials have demonstrated the safety and effectiveness of the Hydrus and iStent. They are multicentre randomised clinical trials. Whilst these are robust studies, they have not provided any insight into the cost analysis nor quality of life changes as a result of these surgical interventions. In fact, there is a scarce resource available on the cost benefit and patient reported outcome measures.
In the current climate within the healthcare system with limited resources even in the most developed part of the world, financing the care can be challenging. Additionally, the finite accessibility to ophthalmic facilities poses a difficulty to policy makers. It is increasingly vital to engage patients in the clinical trial design and including the cost utility analysis of the new procedures and surgical techniques.
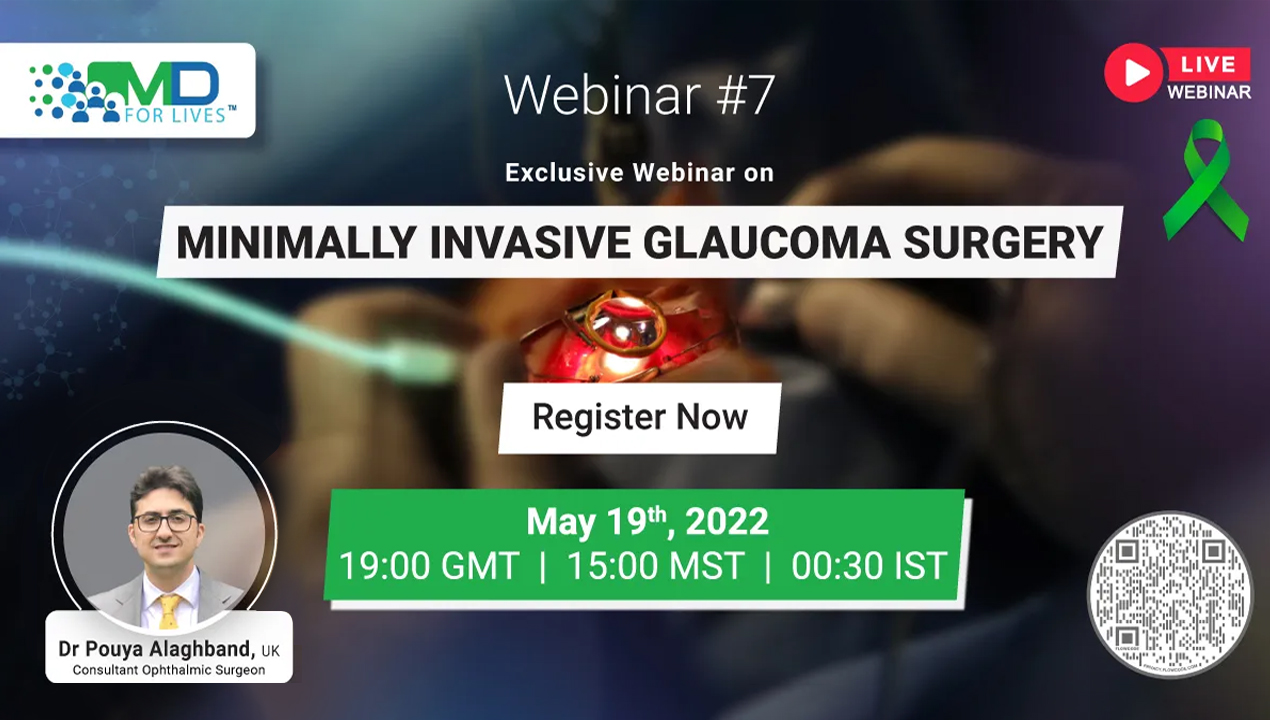
Mr Pouya Alaghband MD(res), PGCert, FRCOphth is a consultant ophthalmic surgeon at the York and Scarborough Teaching Hospital and honorary senior lectures at the Hull York Medical School. He has special interest in glaucoma and has completed his MD(res) at King’s college London on aqueous humour dynamics on MIGS devices. He has been an investigator to some of the landmark studies such as EAGLE, PTVT and commercial trials such as ATHENA and TRITON studies. He is currently the principal investigator for TARGET and CONCEPT trials. He is widely published in the field of the glaucoma and he has presented lectures nationally and internationally. In an online seminar, he will be discussing the history of MIGS, the pivotal clinical trials of some the most commonly used devices such Hydrus, iStent and ECP before exploring the cost benefit and quality of life for the patients within the field. Finally, some of the real world data will be provided to sum up the evidence for these techniques prior to providing the future direction for some of the ongoing clinical trials in the field. There would be an opportunity for question and answers at the end of the meeting.
Lim, K. S. et al. (2008) Mechanism of action of bimatoprost, latanoprost, and travoprost in healthy subjects. A crossover study. Ophthalmology. 115 (5), 790–795.
Quigley, H. A. & Broman, A. T. (2006) The number of people with glaucoma worldwide in 2010 and 2020. The British journal of ophthalmology. 90 (3), 262–267.
Ahmed IIK, Fea A, Au L, Ang RE, Harasymowycz P, Jampel HD, Samuelson TW, Chang DF, Rhee DJ; COMPARE Investigators. A Prospective Randomized Trial Comparing Hydrus and iStent Microinvasive Glaucoma Surgery Implants for Standalone Treatment of Open-Angle Glaucoma: The COMPARE Study. Ophthalmology. 2020 Jan;127(1):52-61. doi: 10.1016/j.ophtha.2019.04.034. Epub 2019 Apr 26. PMID: 31034856.
Ahmed IIK, Rhee DJ, Jones J, Singh IP, Radcliffe N, Gazzard G, Samuelson TW, Ong J, Singh K; HORIZON Investigators. Three-Year Findings of the HORIZON Trial: A Schlemm Canal Microstent for Pressure Reduction in Primary Open-Angle Glaucoma and Cataract. Ophthalmology. 2021 Jun;128(6):857-865. doi: 10.1016/j.ophtha.2020.11.004. Epub 2020 Nov 6. PMID: 33166551.
Trends in Glaucoma Surgeries
Trends in Glaucoma Surgeries Performed by Glaucoma Subspecialists versus Nonsubspecialists on Medicare Beneficiaries from 2008 through 2016
Rathi, Siddarth et al. Ophthalmology, Volume 128, Issue 1, 30 – 38