Researchers have discovered new therapeutic targets for acute myeloid leukemia (AML).
A new study published in Stem Cells suggests transforming growth factor-beta 1 (TGFβ1) can interfere with hematopoiesis, and blocking TGFβ1 can improve hematopoiesis in acute myeloid leukemia (AML).1 Another study led by researchers from Nemours Children’s Health System, US suggests a gene mesothelin expressed in children with AML can be a potential new treatment target for pediatric AML. The study was published in Blood Advances.2
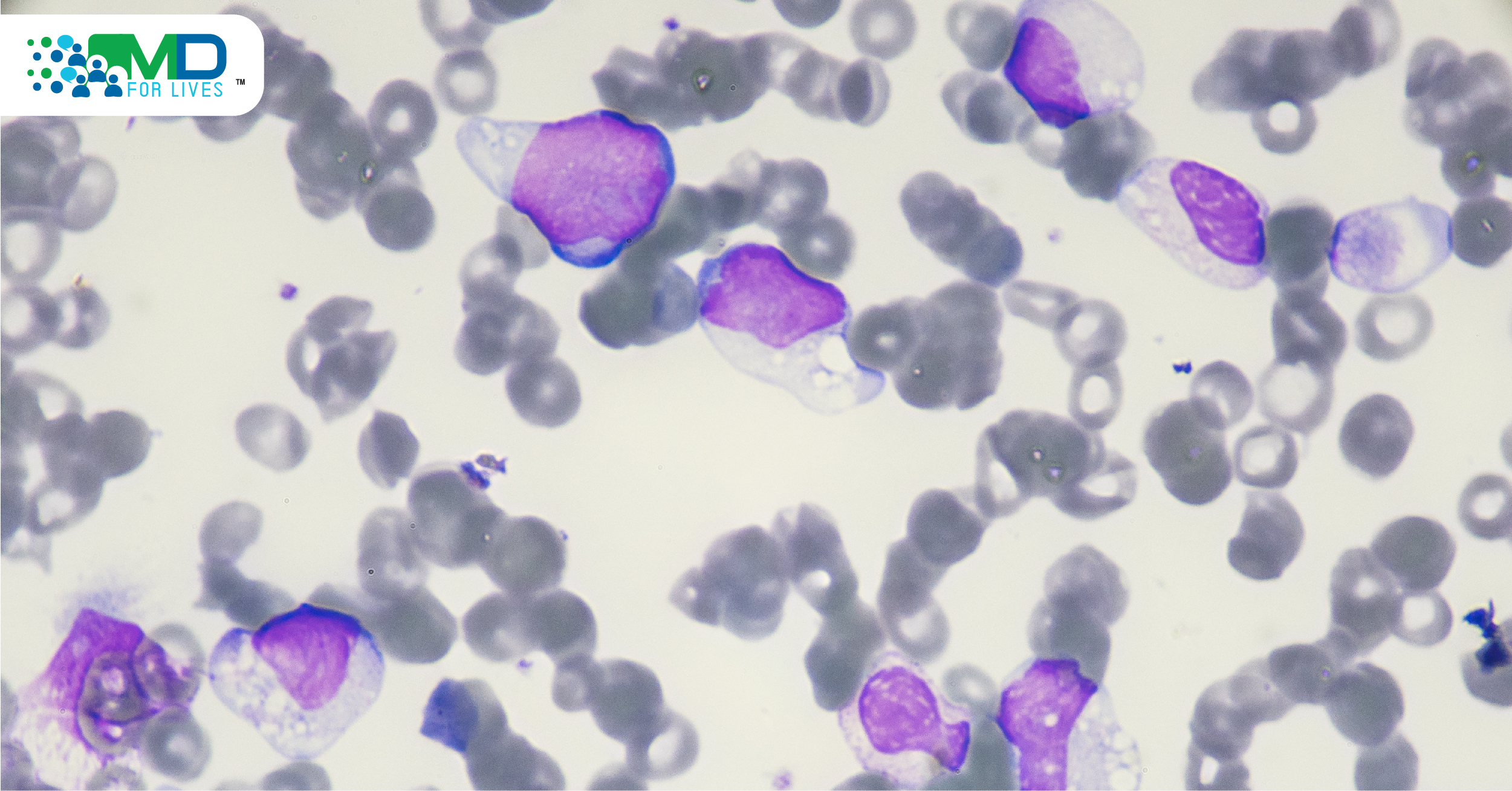
Acute Myeloid Leukemia
Acute myeloid leukemia (AML), the second most common type of leukemia, accounting for approximately 31% of all leukemia diagnosed in adults- according to the American Society of Clinical Oncology.3 It is found that the survival rate for young adults and older varies greatly, younger people have a better prognosis. The estimated 5-year survival rate of AML in people aged 20 and above is 26% and the survival rate below 20 years of age is 68%. AML primarily affects older adults, characterized by poor treatment outcomes.4 The National Cancer Intelligence Network (NCIN) suggests the survival rate in patients above 65 is very poor, approximately 5%.5 The outcome in older patients is explained by the prevalence and the severity of the comorbid conditions and the functional incapacity that increases with age and also the age-related clinical characteristics of the disease.4
Secreted Protein TGFβ1 – Potential New Target to Treat AML
Acute myeloid leukemia (AML), a clinically and genetically heterogeneous disease driven by somatic mutations induces bone marrow failure.6,7 The genetic alteration in hematopoietic stem and progenitor cells (HSPC) leads to the accumulation of poorly differentiated myeloid cells, resulting in functional insufficiency of the hematopoietic system.1 The subsequent cytopenias are associated with adverse clinical outcomes. At diagnosis, almost all patients with AML present with cytopenia, the important cause of morbidity and mortality.
Understanding the underlying mechanism is vital to determine the treatment; however, the mechanism by which AML develops was not completely understood. The previous animal study suggests AML cells induce hematopoietic functional inhibition but the mechanism was not clear.
In a recent study, researchers at Heinrich-Heine-University Düsseldorf exposed the healthy bone marrow-derived CD34+ HSPC to AML-derived cell-free supernatants.1 The results showed significant inhibition in cell proliferation, cell cycling, colony formation and differentiation in the healthy CD34+ HSPC and RNA sequence exhibited specific gene expression signature associated with these inhibitory effects. These functional inhibitions were reflected at the molecular level. Researchers demonstrated overexpression of TGFβ1 in leukemic cells and also the corresponding molecular signature associated with TGFβ1 signaling in healthy CD34+ HSPC. The study suggests pharmacologic inhibition of TGF-β signaling with SD-208 can revert the suppressive effect of TGFβ1.1
The findings indicate that therapeutic targeting of TGF-β may improve hematopoiesis in AML patients.
Mesothelin – A New Treatment Target in Pediatric AML
Acute myeloid leukemia (AML) is a disease of the elderly; however, AML constitutes 15% to 20% of childhood leukemias.8 Despite intensive chemotherapy and allogeneic stem cell transplant, curative therapies for AML remain a significant challenge. Researchers have now shown a new potential path to reduce treatment-related toxicity and improve survival in children with AML.2
Researchers analyzed the transcriptomes of pediatric patients with AML (n=2051) and through genomic sequencing, they compared the expression profile with the normal bone marrow cells. They found the gene mesothelin was highly expressed in one-third (36%) of the patients but absent in normal marrow. Mesothelin, a cell surface protein, is a known therapeutic target in several advanced solid tumors. Besides, it is found the mesothelin expression is particularly high in patients with the extramedullary disease (EMD) and KMT2A gene involvements. Using MSLN-directed ELISA, researchers also confirmed the presence of soluble mesothelin in serum samples, indicating that mesothelin may be used as a diagnostic marker for AML.
Researchers further evaluated the preclinical efficacy of two immunotherapy drugs, anetumab ravtansine (Bayer) and anti-MSLN-DGN462 (ImmunoGen). Both the drugs belong to the mesothelin targeting antibody-drug conjugates (ADCs). ADCs successfully targeted MSLN+ leukemia cell lines in vitro, in vivo, and patient-derived xenograft models. The study demonstrated the overexpression of mesothelin in patients with AML and suggest that mesothelin can be a potential diagnostic biomarker for AML and can also serve as a therapeutic target.2
Both the studies revealed new targets, a promising path to develop new therapeutic strategies for acute myeloid leukemia.

- https://stemcellsjournals.onlinelibrary.wiley.com/doi/full/10.1002/stem.3387
- https://ashpublications.org/bloodadvances/article/5/9/2350/475842/Mesothelin-is-a-novel-cell-surface-disease-marker
- https://www.cancer.net/cancer-types/leukemia-acute-myeloid-aml/statistics
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821042/
- https://www.cancerresearchuk.org/about-cancer/acute-myeloid-leukaemia-aml/survival
- https://www.nejm.org/doi/full/10.1056/NEJMoa074306
- https://www.pnas.org/content/early/2013/07/29/1301891110.abstract