Today, on World Pneumonia Day, MDForLives would like to shed light on something really important – a disease often taken lightly, ‘Pneumonia.’ Most people worldwide view pneumonia as “just another lung infection” that can be treated with antibiotics and rest. But for physicians, it’s a complex condition that requires careful, nuanced care. According to the Global Burden of Disease Study, pneumonia remains one of the most widespread respiratory infections, affecting about 450 million people annually and causing over 3 million deaths worldwide. However, what makes it particularly challenging isn’t just the infection itself but how it interacts with other health issues or ‘comorbidities.’ Hence, while treating pneumonia patients, physicians must recognize that this lung disease doesn’t exist in a vacuum; a string of pneumonia comorbidities tag along!
The presence of pneumonia comorbidities (a list that is way too long!) can significantly impact everything from treatment protocols to recovery timelines. Therefore, healthcare professionals must understand how to manage pneumonia alongside these underlying health conditions for better patient outcomes. In this blog, we have listed out all the comorbidities of pneumonia, how they affect diagnosis and treatment, and why a holistic, personalized approach is essential in delivering the best care.
Identifying the 8 Major Comorbidities of Pneumonia
As of 2024, healthcare researchers have identified eight critical pneumonia comorbidities that can worsen patients’ health by interfering with the standard treatment approach. This, in return, will lead to longer recovery times, more severe symptoms, and a higher risk of complications.
Here’s a rundown of those primary comorbidities of pneumonia that healthcare professionals should be aware of:
Chronic Obstructive Pulmonary Disease (COPD)
Patients with COPD are at a significantly higher risk of developing pneumonia, especially during acute exacerbations of their condition. COPD weakens the lungs’ defenses, making it easier for pathogens to cause infection.
In turn, pneumonia can worsen COPD symptoms, leading to more frequent hospitalizations and a greater risk of respiratory failure.
Heart Disease
Cardiovascular disease, particularly hypertension, is a well-documented risk factor that can lead to worse outcomes in pneumonia cases. In these patients, pneumonia can exacerbate cardiac dysfunction, leading to arrhythmias, fluid overload, or even heart failure exacerbation.
Diabetes Mellitus
Diabetes weakens the immune system, making individuals more susceptible to infections, including pneumonia. Elevated blood glucose levels can impair the body’s ability to fight infections and may delay recovery.
Moreover, uncontrolled diabetes is linked to worse outcomes in pneumonia patients, including prolonged hospital stays and higher mortality rates.
Renal Impairment
Patients with Chronic Kidney Disease (CKD) or Acute Kidney Injury (AKI) face more significant challenges when battling pneumonia. Renal impairment complicates antibiotic metabolism and excretion, which can lead to drug toxicity or underdosing.
Cancer
Cancer patients, especially those undergoing chemotherapy or radiation therapy, have a weakened immune system. This makes them vulnerable to respiratory infections.
Pneumonia in cancer patients can be more challenging to treat due to immunosuppression, drug interactions, and the potential for pneumonia to mask cancer-related symptoms.
HIV/AIDS
Immunocompromised patients, such as those living with HIV/AIDS, are at an increased risk of developing pneumonia, particularly opportunistic infections like Pneumocystis jirovecii pneumonia (PCP).
These infections often present differently than typical bacterial pneumonia and require specialized treatment.
Liver Disease
Patients with chronic liver disease, especially those with cirrhosis, are at a heightened risk of developing pneumonia.
Liver dysfunction impairs the immune response. It decreases protein production in the body’s defense mechanisms. This makes patients more susceptible to infections.
Obesity
Obesity is a growing global health concern that predisposes individuals to a wide array of health issues, including pneumonia.
Obese individuals are more likely to suffer from hypoventilation and have a reduced ability to clear respiratory pathogens, which makes pneumonia more severe and more complex to treat.
Impact Of Comorbidities on Pneumonia Outcomes
Comorbidities significantly worsen pneumonia outcomes, amplifying the severity and complexity of the disease in numerous ways.
Here’s a closer look at the critical impacts of pneumonia comorbidities:
1. Increased Mortality Rates
Patients with comorbid conditions are at a higher risk of mortality from pneumonia. Research indicates that having even one additional health condition can increase the risk of death. The more health conditions a person has, the higher the risk becomes.
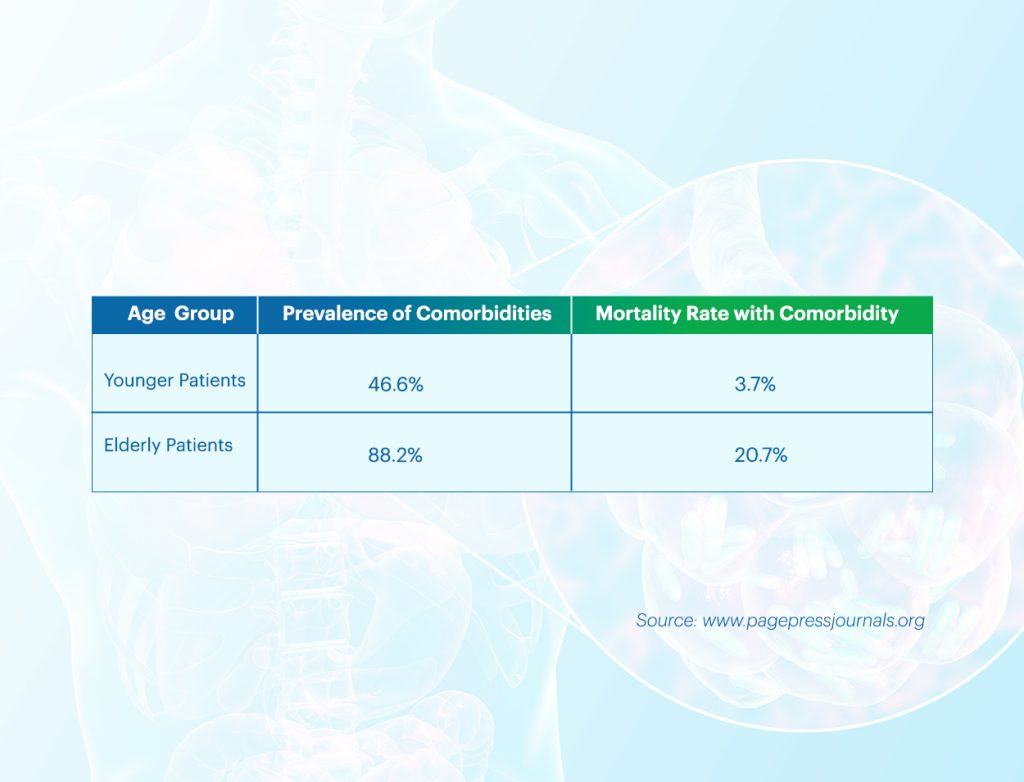
Pneumonia comorbidities, especially – heart failure, chronic kidney disease, and diabetes, interfere with the body’s ability to recover from infections, resulting in poorer prognosis and higher mortality rates.
2. Length of Hospital Stay and Recovery Time
Comorbidities of pneumonia also contribute to extended hospital stays and slower recovery times.
Patients with respiratory or cardiovascular diseases often require intensive monitoring, longer courses of antibiotics, and more complex care protocols. Their recovery is slower due to the compounded effect of the infection and the strain on other organs.
3. Risk of Complications
The risk of complications like respiratory failure, sepsis, and organ dysfunction is higher in patients with pneumonia comorbidities.
For example, a diabetic patient with pneumonia may experience poor wound healing and a weakened immune response, making infections more severe and complex to treat.
Similarly, cardiovascular diseases can exacerbate the strain pneumonia places on the heart and lungs, increasing the likelihood of severe complications.
Managing Pneumonia in Patients with Comorbidities
For physicians, managing pneumonia in patients with comorbidities requires a holistic approach that goes beyond standard pneumonia treatment. Here are some critical areas to consider:
- Personalized Care Plans: Every patient with pneumonia needs a treatment plan that considers their unique health profile, especially when they have existing health issues. A “one-size-fits-all” approach won’t work with patients with any of the eight pneumonia comorbidities mentioned above in this blog. Physicians should evaluate each patient’s risk factors for pneumonia and tailor treatment plans accordingly. This could mean adjusting medication doses, choosing antibiotics more selectively, or engaging additional specialists to ensure comprehensive care.
- Early Detection and Proactive Monitoring: For high-risk patients, catching pneumonia early can be the difference between a mild case and a severe complication. Physicians can adopt proactive measures such as regular screening, especially during peak pneumonia seasons. Being alert to symptoms and changes in patients with pneumonia comorbidities helps ensure early intervention, which can reduce the severity of pneumonia and prevent it from escalating.Continuous monitoring is also vital, as high-risk patients may experience sudden changes in their condition. Monitoring tools like pulse oximeters or other digital health trackers can help physicians and patients track essential signs and catch potential issues early.
- Multidisciplinary Care and Coordination: Managing pneumonia in patients with comorbidities often requires a team-based approach. Involving other specialists, such as cardiologists, endocrinologists, and pulmonologists, can help tailor treatment to each patient’s needs. This team-based approach allows for better management of the patient’s primary condition alongside pneumonia, resulting in a more seamless and effective treatment process.
Preventive Measures: The Power of Vaccination and Beyond
Vaccination remains a cornerstone in pneumonia prevention, particularly important for high-risk populations. It significantly lowers the incidence and severity of both bacterial and viral respiratory infections.

Critical vaccines, like the pneumococcal vaccines (PCV13 and PPSV23), protect against Streptococcus pneumoniae, a common cause of bacterial pneumonia. The flu vaccine also helps by reducing the chance of pneumonia that can follow a viral infection.
Please note: Since flu and pneumococcal infections often go hand-in-hand, getting both vaccines is highly recommended for older adults, people with weakened immune systems, and those with chronic conditions to reduce the risk of hospitalizations and complications.
Studies show that the pneumococcal vaccine reduces the risk of invasive pneumococcal disease by up to 75% in older adults and high-risk individuals. Influenza vaccines, which lower the chances of secondary bacterial infections, have also been shown to decrease hospitalizations related to pneumonia and influenza by nearly 40% in older patients.
In addition to immunization, clinicians can counsel patients suffering from comorbidities of pneumonia on evidence-based lifestyle modifications that enhance systemic resilience. Smoking cessation is particularly critical, as smoking impairs mucociliary clearance and immune defenses, increasing susceptibility to respiratory infections. Furthermore, a nutrient-dense diet and regular physical activity contribute to better immune response and improved lung function, creating a more robust defense against pneumonia pathogens.
Education on early symptom recognition, such as persistent cough, dyspnea, or chest discomfort, can empower patients to seek timely care, potentially averting progression to severe pneumonia. Prophylactic antibiotic regimens may be indicated for specific high-risk individuals to reduce recurrent respiratory infections.
However, these must be prescribed judiciously to avoid antibiotic resistance and are typically reserved for patients with underlying respiratory conditions or those with repeated episodes of bacterial pneumonia.
Involve Patients in their Healthcare Journey
‘Patient education’ is an integral part of managing patients with comorbidities of pneumonia. When patients understand the risks associated with their conditions, they’re more likely to take preventive measures seriously.
Physicians can encourage patients to get vaccinated, adopt healthier habits, and take their symptoms seriously, empowering them to participate actively in their healthcare journey.
This can be as simple as educating them about symptoms of pneumonia to watch for or explaining why consistent medication adherence matters to treat pneumonia comorbidities.
Holistic Care for Patients with Pneumonia Comorbidities
This is a gentle reminder that pneumonia is no small challenge for patients with comorbidities.
It’s a severe health issue that requires comprehensive care.
As the number of individuals with pneumonia comorbidities continues to grow, a holistic approach to pneumonia care is essential, especially as we observe World Pneumonia Day.
Comorbidities of pneumonia, such as diabetes, heart disease, chronic lung disorders, etc., can make pneumonia harder to treat, leading to missed opportunities for prevention, extended recovery times, and more severe complications.
Integrating chronic disease management with acute pneumonia care allows healthcare providers to tailor treatments to each patient’s unique needs better, ultimately leading to fewer hospitalizations and faster recovery. We believe this approach can significantly improve patient outcomes and offer a more effective pathway to healing.
Join MDForLives to contribute your expertise through paid medical surveys and gain insight into critical issues such as comorbidities of pneumonia.
You can also share your case studies with us at collaboration@mdforlives.com and earn up to $100!

The creative force behind the keyboard, Pallabi crafts narratives of healthcare wonders and research marvels. As a seasoned professional blogger, she ventures to unearth the riches of medical innovation, weaving them into insightful stories that educate.